15 Male Reproductive System
Learning Objectives
- Identify the anatomy of the male reproductive system
- Describe the main functions of the male reproductive system
- Spell the male reproductive system medical terms and use correct abbreviations
- Identify the medical specialities associated with the male reproductive system
- Explore common diseases, disorders, and procedures related to the male reproductive system
Chapter Fifteen: Table of Contents
What Can Go Wrong? – Diseases, Disorders, and Conditions of the Male Reproductive System
- Male Breast
- Testes and Epididymis
- Prostate Gland
- Penis
- Sexually Transmitted Diseases – STDs (Not specific to males)
How Do We Fix it or Make it Better?
Reproductive System
| Term | Word Breakdown | Description |
|---|---|---|
| prostrate gland | Produces a milky fluid that nourishes and protects sperm. | |
| testis tE-steez |
Male reproductive organs responsible for producing sperm and testosterone. | |
| epididymitis ep-uh-dId-uh-muhs |
A tubular structure on the testis where sperm matures. Read more | |
| penis pEE-nuhs |
External male reproductive organ involved in sexual intercourse and urination. | |
| vas deferens vAs |
Responsible for transporting sperm from the epididymis to the ejaculatory ducts. The sperm travels through the prostrate and empties into the urethra | |
| sperm spUHRm |
Male gametes necessary for fertilization. | |
| semen sEE-muhn |
The fluid that contains sperm and other seminal components. | |
| spermatogeneis | The process of sperm production. | |
| testes (testicles) | Testes (testicles). The testes are 2 small organs that are found inside the scrotum. The testes are responsible for making sperm and are also involved in producing a hormone called testosterone. Read more |
Gametes are the reproductive cells that combine to form a fetus. Organs called gonads produce the gametes, along with the hormones that regulate human reproduction. The male gametes are called sperm. Spermatogenesis occurs within the seminiferous tubules that make up most of the testis. The scrotum is a sac that holds the testes outside of the body cavity.
Return to the Table of Contents
Male Reproductive System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Male Reproductive System.
Watch this video:
Media 9.1. Reproductive System, Part 2 – Male Reproductive System: Crash Course A&P 41 [Online video]. Copyright 2015 by CrashCourse.
Male Reproductive System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Male Reproductive System.
Male Reproductive Medical Terms
Anatomy (Structures) of the Male Reproductive System
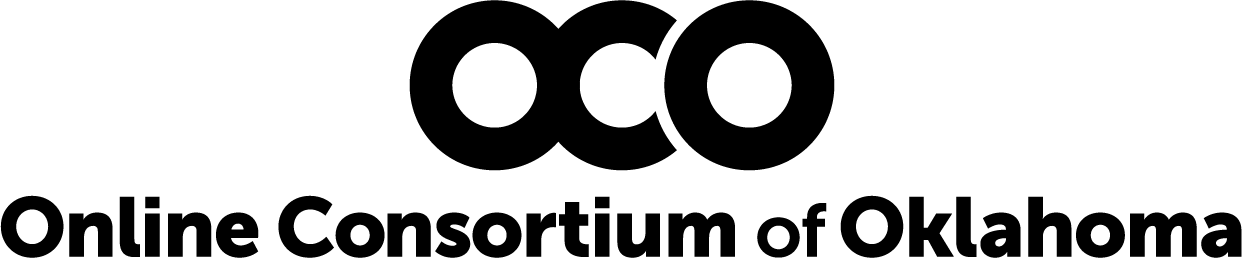
The structures of the male reproductive system include the testes, the epididymis, the penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the vas deferens. The spermatic cord is an enclosed sheath which includes the vas deferens, arteries, veins and nerves. The seminal vesicles and prostate gland add fluids to the sperm to create semen .
Return to the Table of Contents
Physiology (Function) of the Male Reproductive System
Spermatogenesis
Spermatogenesis occurs in the seminiferous tubules that form the bulk of each testis. The process begins at puberty, after which time sperm are produced constantly throughout a man’s life. One production cycle takes approximately 64 days. One production cycle is considered from spermatogonia through to formed sperm. A new cycle starts approximately every 16 days, although this timing is not synchronous across the seminiferous tubules.
Sperm
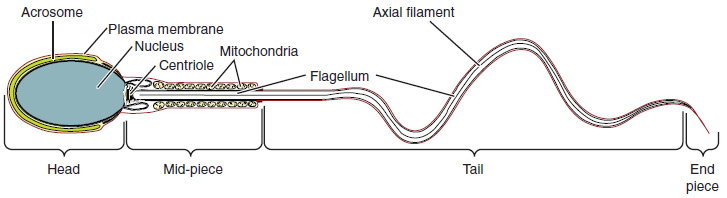
Sperm are smaller than most cells in the body; in fact, the volume of a sperm cell is 85,000 times less than that of the female gamete. Approximately 100 to 300 million sperm are produced each day, whereas women typically ovulate only one oocyte per month as is true for most cells in the body, the structure of sperm cells speaks to their function. Sperm have a distinctive head, mid-piece, and tail region (see Figure 9.2).
Sperm Transport
To fertilize an egg, sperm must be moved from the seminiferous tubules in the testes, through the epididymis, and—later during ejaculation—along the length of the penis and out into the female reproductive tract. It takes an average of 12 days for sperm to move through the coils of the epididymis, with the shortest recorded transit time in humans being one day.
Epididymis
Sperm enter the head of the epididymis and are moved by the contraction of smooth muscles lining the epididymal tubes. As the sperm mature they acquire the ability to move under their own power. Once inside the female reproductive tract, they will use this ability to move independently toward the unfertilized egg. The more mature sperm are then stored in the tail of the epididymis until ejaculation occurs.
Ducts
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the vas deferens (also called the ductus deferens). The vas deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord. From each epididymis, each vas deferens extends through the inguinal canal in the abdominal wall and continues to a region called the ampulla. The sperm is mixed with fluid from the paired seminal vesicles and moves into its associated ejaculatory duct. The ejaculatory ducts transport the seminal fluid to the prostate gland.
Prostate Gland
The prostate gland secretes an alkaline, milky fluid to the passing seminal fluid (referred to as semen) to first coagulate and then decoagulate the semen following ejaculation. The temporary thickening of semen helps retain it within the female reproductive tract and once decoagulated the sperm can pass farther into the female reproductive tract.
Bulbourethral Glands
Bulbourethral glands release a thick, salty fluid that lubricates the end of the urethra and vagina, and helps to clean urine residues from the penile urethra.
Concept Check
- Write or draw out the components of the pathway that sperms takes from beginning until the end.
- Consider fertility challenges that may be experienced if a large number of defective sperm are produced.
Return to the Table of Contents
Anatomy Labeling Activity
Return to the Table of Contents
Male Reproductive Terms not Easily Broken into Word Parts
Return to the Table of Contents
Common Male Reproductive System Abbreviations
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Male Reproductive System
Diseases, Disorders, and Conditions of the Male Breast
| Term | Word Breakdown | Description |
|---|---|---|
| gynecomastia gie-nuh-koh-mAs-tee-uh |
-ia condition gynec/o mast/o |
Enlargement of male breast tissue. |
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Testes and Epididymis
| Term | Word Breakdown | Description |
|---|---|---|
| cryptorchism krip-tOR-kiz-uhm |
-ism condition crypt/o orch/o |
A condition where one or both testicles fail to descend into the scrotum |
| epididymitis ep-uh-did-uh-mIE-tuhs |
-itis inflammation epi- didym/o |
Inflammation of the epididymis. The epididymis Serves as a site for sperm maturation and storage Read more |
| oligospermia | -ia condition oligo- spermat/o |
Condition of low sperm count |
| orchitis | -itis inflammation orch/o |
Pain and swelling of a testes National Library of Medicine |
| seminoma | -oma tumor; mass; fluid collection semin/o |
A type of testicular cancer. |
| varicocele vAr-uh-koh-seel |
-cele bulge; hernia varic/o |
Condition characterized by enlarged and twisted veins in the scrotum |
Testicular cancer begins in the testicle or testis. It is most often found in men age 15 to 44 years, although it can be diagnosed at any age (Canadian Cancer Society, 2020). Testicular cancer is rare and treatable when diagnosed early. Common symptoms are a painless lump in the testicle, swelling, a heavy feeling in the scrotum or abdomen, amongst others. Sometimes, testicular cancer is found during infertility testing. An orchiectomy is the most common procedure for diagnosing and treating testicular cancer (Canadian Cancer Society, 2020). To learn more about testicular cancer, diagnosis and treatments please go to the Canadian Cancer Society’s web page on testicular cancer.
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Prostrate Gland
| Term | Word Breakdown | Description |
|---|---|---|
| benign prostatic hypertrophy (BPH) bi-nIEn prah-stAt-ikhie-pUHR-truh-fee |
prostat/o prostrate -trophy hyper- |
A condition in which the prostate gland is enlarged and not cancerous. Benign prostatic hyperplasia is also called benign prostatic hypertrophy or benign prostatic obstruction. It can pinch the urethra making it difficult to empty the bladder resulting in the need to urinate frequently, especially at night. National Institutes of Health |
| prostatitis prah-stuh-tIE-tuhs |
-itis inflammation prostat/o |
Inflammation of the prostate National Institutes of Health |
Prostate Cancer
According to the Centers for Disease Control and Prevention (CDC), prostate cancer is the second most common cancer occurring in men. However, some forms of prostate cancer grow very slowly and may not require treatment. Aggressive forms of prostate cancer, in contrast, involve metastasis to organs like the lungs and brain. There is no link between Benign Prostatic Hyperplasia and prostate cancer, but the symptoms are similar. Prostate cancer is detected by medical history, a blood test, and a digital rectal exam that allows physicians to palpate the prostate and check for unusual masses. If a mass is detected, the cancer diagnosis is confirmed by biopsy of the cells (Betts, et al., 2013).
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Penis
| Term | Word Breakdown | Description |
|---|---|---|
| balanitis | -itis inflammation balan/o |
Inability to retract the foreskin of the penis |
| dyspareunia | -ia condition dys- pareun/o |
Difficult or painful sexual intercourse |
| phimosis | -osis condition |
A condition characterized by the narrowing of the opening of the foreskin. |
| priapism prIE-uh-piz-uhm |
-ism condition |
an abnormal often painful persistent erection of the penis |
Return to the Table of Contents
Erectile Dysfunction Disorder (EDD)
Erectile dysfunction (ED) is a condition in which a male has difficulty either initiating or maintaining an erection. The combined prevalence of minimal, moderate, and complete ED is approximately 40% in men at age 40 and reaches nearly 70% by 70 years of age. In addition to aging, ED is associated with diabetes, vascular disease, psychiatric disorders, prostate disorders, the use of some drugs such as certain antidepressants, and problems with the testes resulting in low testosterone concentrations. These physical and emotional conditions can lead to disruptions in the vasodilation pathway and result in an inability to achieve an erection (Betts, et al., 2013).
Sexually Transmitted Diseases
| Term | Word Breakdown | Description |
|---|---|---|
| chlamydia kluh-mId-ee-uh |
A sexually transmitted bacterial infection that has relatively few symptoms which is why it is known as the "silent infection." Even though the symptoms maybe absent or mild, it can lead to reproductive problems in females. If symptoms are present thy include discharge from the vagina or penis, and a burning sensation when urinating. CDC Chlamydia. | |
| genital herpes jEn-uh-tl hUHR-peez |
A sexually transmitted disease caused by the herpes simplex virus. Causes small blisters on or around the genitals, rectum, or mouth. It can be managed, but not cured. CDC Genital Herpes | |
| genital warts (HPV) jEn-uh-tl wORts |
Genital warts caused by the Human Papilloma virus. If left untreated, the warts are associated with cervical cancer.CDC- Human Papillomavirus (HPV) | |
| gonorrhea gah-nuhr-rEE-uh |
A sexually transmitted disease (STD) caused by a bacterial infection. Gonorrhea infects the mucous membranes of the reproductive tract, including the cervix, uterus, and fallopian tubes in women, and the urethra in women and men. It can cause a greenish-yellow discharge from the urethra or vagina. The disease is treatble.CDC - Gonorrhea | |
| syphilis sIf-uh-luhs |
Sexually transmitted bacterial infection that causes chancre (SHANG - kur) which is a small sore. If it is not treated the disease progresses and can become life threatening, CDC - Syphilis | |
| trichomoniasis trik-uh-muh-nIE-uh-suhs |
Common STD that comes from a parasite. The symptoms are itching and discomfort during urination. and in females, a fishy smell. It is treatable. Trichomoniasis – CDC Basic Fact Sheet |
The terms for sexually transmitted infections (STI) and sexuality transmitted diseases (STD) are often used interchangeably. Sexuality transmitted disease (STD) implies the disease was acquired through sexual transmission. A disease is a disorder of structure or function in a human, which produces specific signs or symptoms. A disease must be managed, as with the case of human immunodeficiency virus (which can also be acquired through the transmission of other bodily fluids; thus not solely sexual transmission). The treatment may include antiretrovirals or anti-virals (Urology Care Foundation, 2019).
Chlamydia (CT)
Chlamydia is one of the most common sexually transmitted infections (STIs) caused by bacteria that infect the cervix, urethra and other reproductive organs. Chlamydia is easy to treat and can be cured. Many people with chlamydia do not have any symptoms and unknowingly pass the infection to their sexual partner(s). If symptoms develop, they usually appear two to six weeks after sexual contact with an infected person. Males may have penial discharge and itching around the urethra. The urethra is the opening in the penis. Males may also experience dysuria , polyuria , urethral pain and urethritis (Ontario Agency for Health Protection and Promotion , 2019; Region of Peel, 2007).
Chlamydia spreads through unprotected oral, anal or vaginal sex with an infected person. Chlamydia can be spread to the eyes via the hands with direct contact of infected fluids. Until a patient finishes their treatment, they continue to have the infection and can continue to pass it to others. Chlamydia is treated with antibiotic pills. If the patient has epididymitis, they may need to be hospitalized and be treated with intravenous (IV) antibiotics. All sexual partners within the past 60 days should be examined, treated, and informed that having no symptoms does not mean there is no infection (Ontario Agency for Health Protection and Promotion, 2019; Region of Peel, 2007).
Gonorrhea (Gonococcus) – (GC)
Gonorrhea is a sexually transmitted infection (STI) caused by bacteria that infects the cervix, urethra and other reproductive organs. Infections can also infect the throat and anus. Gonorrhea can be treated and cured. Many people infected with gonorrhea have no symptoms and can unknowingly pass the infection on to their sexual partner(s). If symptoms develop, they may appear two to seven days after sexual contact with an infected person. Symptoms vary depending on which part of the body is infected. Males may have yellowish-white discharge from the penis. They may also have dysuria , polyuria , testicular pain and testitis . Gonorrhea infection from oral sex may lead to sore throat and swollen glands. Gonorrhea infection from anal sex may cause itchiness and discharge from the anus. Gonorrhea is spread through unprotected oral, vaginal or anal sex with an infected person. Until the patient finishes their treatment, they continue to have the infection and can pass it to others (Ontario Agency for Health Protection and Promotion, 2019a; Region of Peel, 2007).
Gonorrhea is treated with oral antibiotics in combination with an intramuscular (IM) injection. It is important that one completes the treatment and abstain from unprotected sexual activity for at least seven days following treatment. If the patient develops epididymitis, the patient may need to go to a hospital and be treated with intravenous antibiotics.
All sexual partners within the past 60 days should be examined, treated and informed that having no symptoms does not mean there is no infection (Ontario Agency for Health Protection and Promotion, 2019a; Region of Peel, 2007).
Reportable Diseases
Both chlamydia and gonorrhea are reportable diseases to the Ministry of Health and Long Term Care. Therefore, the local health department will be calling the doctor’s office or patient to ensure correct treatment was received and sexual partners have been followed up with testing and treatment (Ontario Agency for Health Protection and Promotion, 2019a; Region of Peel, 2007). To learn more about STIs and STDs such as chlamydia and gonorrhea please go to the Public Health Ontario website.
Human Papillomavirus- HPV
HPV is another common sexually transmitted infection (STI). Both males and females can be infected with HPV. Around three quarters of sexually active individuals have been exposed to HPV during their lifetime. There are over 100 strains of HPV and some strains of HPV can cause visible genital warts. The warts are usually painless but may be itchy, uncomfortable and hard to treat. Some strains of HPV cause genital, anal, throat and cervical cancers. HPV spreads through sexual activity and skin-to-skin contact in the genital area with an infected person. Since some people are asymptomatic they don’t know they have the virus and consequently pass the virus to their sexual partners. Treatments are available for genital warts but there is no cure for HPV (York Region Health Connect, n.d.). To learn more about HPV symptoms, treatments, and prognosis visit the York Region Fact Sheet (PDF file) on HPV.
HPV Vaccine
A vaccine called Gardasil® 9 is available for 9 HPV strains. This vaccine assists the immune system in protecting the body against infections and diseases caused by HPV (York Region Health Connection, n.d.). To learn more about Gardasil® 9 treatments, please visit the Gardasil® 9 website.
Herpes Simplex Virus (HSV)
Genital herpes is a sexually transmitted infection (STI) that is caused by a virus called herpes simplex virus (HSV). There are two types of herpes simplex viruses:
- Type 1- oral herpes or cold sores (HSV-1)
- Type 2- genital herpes (HSV-2).
These viruses are very similar and either type can cause genital herpes or cold sores. Symptoms might include dysuria, enlarged glands, myalgia, arthralgia and fever. Once a patient is infected with HSV, the virus remains in their body even after the symptoms are gone and can cause recurring outbreaks. When the virus becomes active again, the symptoms return but are usually less painful and heal faster. Recurring outbreaks vary from person-to-person, however they can be triggered by emotional or physical stress, exposure to sunlight, hormonal changes, poor nutrition, sexual intercourse, lack of sleep or a low immune system.
Herpes is spread through direct contact with the sores or blisters of an infected person. Contact (and transfer of the virus) can occur from genitals-to-genitals, mouth-to-genitals or mouth-to-mouth. Herpes can also be passed to the anal area. Herpes spreads easily during sexual contact while symptoms are present, or just before an outbreak of symptoms. An infected person may spread herpes even when they have no symptoms; this is called asymptomatic shedding. One can spread the herpes virus to other parts of their body after touching the sores; autoinoculation. The fingers, eyes and other body areas can accidentally become infected in this way. Hand washing after touching sores and blisters is recommended to prevent spreading the virus.
There is no cure for herpes. Antiviral pills help to reduce symptoms and speed the healing of blisters or sores and are prescribed by a doctor. Treatment of symptoms may be managed with medication for pain, bath salts, cold compresses and urinating in water may help to relieve discomfort. Keep the infected area clean and dry, wear cotton underwear and loose clothing to reduce discomfort. All sexual partner(s) should be informed. The only way to reduce the risk of transmission of herpes is to avoid direct contact with the sores and to use condoms. Condoms will reduce but not eliminate risk as the virus can be present and shed from the skin in the genital area (Ontario Ministry of Health and Long-Term Care, 2015).
To learn more about the symptoms, complications, treatments and prognosis of HSV please visit the Ontario Ministry of Health and Long-Term Care’s Sexually Transmitted Diseases : Genital Herpes website or Public Health Ontario’s Testing Index.
STD/STI Medical Abbreviations
Return to the Table of Contents
Medical Terms in Context
Return to the Table of Contents
Male Reproductive System: Laboratory and Diagnostic Procedures
| Term | Word Breakdown | Description |
|---|---|---|
| Blood Test prostate specific antigen (PSA) |
Screening for prostate cancer. A High PSA can be associated with prostate cancer as well as other prostrate problems. High PSA counts may indicate a need for biopsy. | |
| Semen Analysis azoospermia |
-ia condition a- without lacking zo/o |
Semen that contains no sperm |
| Semen Analysis morphology mor-fAH-luh-jee |
-ology study of morph/o |
The study of size and shape of the sperm. Medline Plus Semen Analysis |
| Semen Analysis motility moh-tIl-uh-tee |
The study of the movement of the sperm Medline Plus Semen Analysis |
|
| digital rectal examination – (DRE) | A digital rectal exam is an exam of the lower rectum. The health care provider uses a gloved, lubricated finger to check for any abnormal findings. In men, the test can be used to check the size of the prostate and to look for abnormal bumps or other changes of the prostate gland. A digital rectal exam may also be done to collect stool for testing for fecal occult (hidden) blood as part of screening for cancer of the rectum or colon. Medline Plus Digital rectal exam | |
| testicular self-examination (TSE) | A testicular self-exam (TSE) is an easy way for males to check their own testicles to make sure there aren't any unusual lumps or bumps - which can be the first sign of testicular cancer. Read More |
Return to the Table of Contents
Male Reproductive System: Surgical Procedures
| Term | Word Breakdown | Description |
|---|---|---|
| circumcision sUHR-km-sizh-uhn |
-ion process circum- |
Procedure that involves the surgical removal of the foreskin from the penis |
| orchiectomy or-kee-Ek-tuh-mee |
-ectomy cut out; surgical removal orchi/o |
The surgical removal of one or both testicles |
| orchiopexy | -pexy surgical fixation orchi/o |
A surgical procedure to move undescended testicles into the scrotum |
| prostatectomy prah-stuh-tEk-tuh-mee |
-ectomy cut out; surgical removal prostat/o |
The surgical removal of the prostate gland |
| vasectomy vuh-sEk-tuh-mee |
-ectomy cut out; surgical removal vas/o |
Surgical procedure in which the vas deferens, the tube that carries sperm from the testicles to the urethra, is cut or blocked. This procedure is considered a permanent form of male contraception and prevents the release of sperm during ejaculation |
| vasovasostomy | -ostomy the surgical creation of new opening (to form a mouth) vas/o |
Reversal of a vasectomy. The vas deferens is reopened after a vasectomy |
Vasectomy
Return to the Table of Contents
Watch the Animated Dissection of Anatomy for Medicine’s (A.D.A.M.) video to learn about a vasectomy. As described in this video, a vasectomy is a procedure in which a small section of the ductus (vas) deferens is removed from the scrotum. This cuts off the path taken by sperm through the ductus deferens. (as cited in Betts, et al., 2013).
No-Scalpel Vasectomy (NSV)
An alternative to a traditional vasectomy is the no-scalpel vasectomy (NSV). This is a minimally invasive procedure and an added benefit is that the recovery time is shorter. All vasectomies are completed by a urologist (Gentle Procedures Clinic, n.d.). To learn more about the NSV procedure, visit No-Scalpel Vasectomy Procedure Info by the Gentle Procedures Clinic in Toronto, Ontario.
Medical Specialties
Urology
Urology is a surgical sub specialty in which the surgeon has additional training in the treatments of diseases and disorders of the male and female urogenital systems (Canadian Medical Association, 2018). To learn more about urology and the training involved to become a urologist visit the Canadian Medical Association’s Urology Profile.
Return to the Table of Contents
References
Canadian Cancer Society. (2020). Symptoms of testicular cancer. https://www.cancer.ca/en/cancer-information/cancer-type/testicular/signs-and-symptoms/?region=on
Canadian Medical Association. (2018). Urology Profile. https://www.cma.ca/sites/default/files/2019-01/urology-e.pdf
CrashCourse. (2015, November 9). Reproductive system, part 2 – Male reproductive system: Crash course A&P 41. YouTube. https://youtu.be/-XQcnO4iX_U
Gentle Procedures Clinic. (n.d). No-Scalpel vasectomy procedure info. https://gentleprocedurestoronto.ca/vasectomy/no-scalpel-no-needle/
Ontario Agency for Health Protection and Promotion. (2019). Chlamydia. Public Health Ontario. https://www.publichealthontario.ca/en/diseases-and-conditions/infectious-diseases/sexually-transmitted-infections/chlamydia
Ontario Agency for Health Protection and Promotion. (2019a). Gonorrhea. Public Health Ontario. https://www.publichealthontario.ca/en/diseases-and-conditions/infectious-diseases/sexually-transmitted-infections/gonorrhea
Ontario Ministry of Health and Long-Term Care. (2015). Sexually transmitted diseases: Genital herpes (hur-peez). Publications. http://www.health.gov.on.ca/en/public/publications/std/herpes.aspx
Region of Peel. (2007). Chlamydia and Gonorrhea. https://www.peelregion.ca/health/talk-to-me/download/lesson-plans/lesson6-pdf/lesson6i.pdf
Urology Care Foundation. (2019). What are sexually transmitted infections (STIs) or diseases (STDs)?. https://www.urologyhealth.org/urologic-conditions/sexually-transmitted-infections#Acquired_Immune_Deficiency_Syndrome_(AIDS)
York Region Health Connection. (n.d.). Human Papillomavirus: https://www.york.ca/wps/wcm/connect/yorkpublic/b5158069-a667-4f43-bb25-e0449ba22caa/6052+Human+Papilloma+Virus+Fact+Sheet.pdf?MOD=AJPERES&CACHEID=b5158069-a667-4f43-bb25-e0449ba22caa
Return to the Table of Contents
Image Descriptions
Figure 9.1 image description: This figure shows the different organs in the male reproductive system. The top panel shows the side view of a man and an uncircumcised and a circumcised penis. The bottom panel shows the lateral view of the male reproductive system and the major parts are labeled. [Return to Figure 9.1].
Figure 9.2 image description: This diagram shows the structure of sperm; the major parts are labeled (from left to right): head section (acrosome, plasma membrane, nucleaus), mid-piece (centriole, mitochondria, flagellum), tail (flagellum, axial filament), end piece (end piece). [Return to Figure 9.2].
Return to the Table of Contents
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
haploid reproductive cells that contribute genetic material to form an offspring
reproductive organs (testes in men and ovaries in women) that produce gametes and reproductive hormones
Process of producing sperm
tube structures within the testes where spermatogenesis occurs
external pouch of skin and muscle that houses the testes
male gonads (singular = testis)
Blood vessels that transport blood away from the heart.
Blood vessels that carry blood back to the heart.
Collection of neurons; nerve cells
doughnut-shaped gland at the base of the bladder surrounding the urethra and contributing fluid to semen during ejaculation
male gamete (spermatozoon)
ejaculatory fluid composed of sperm and secretions from the seminal vesicles, prostate, and bulbourethral glands
diploid precursor cells that become sperm (singular = spermatogonium)
female gamete
(plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation
Pertaining to the epididymis
(also, ductus deferens) duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred as the vas deferens
(also, Cowper’s glands) glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation
male gonad (testes=plural)
Excision/removal of the testicle.
Cancer spreads from one part of the body into another
treatment that works against the virus replication
treatments that work effectively against a virus.
painful urination
frequent urination
inflammation of the urethra
swelling of the epididymis
Inflammation of the testicles
Antiobiotics are medications that stop bacterial infections.
pertaining to within the muscle
pertaining to without symptoms
pain in the muscles
painful joint(s)
self inoculation