5 Digestive System
Learning Objectives
- Identify general terms related to the digestive system
- Spell the digestive system medical terms and use correct abbreviations
- Identify the medical specialties associated with the digestive system
- Recognize common diseases, disorders, and procedures related to the digestive system
Chapter Five: Table of Contents
What is it? – General Terms: Digestive System
What Can Go Wrong? – Diseases, Disorders, and Conditions
- Mouth, Lips Tongue, and Gums
- Esophagus, Stomach, and Abdominal Cavity
- Small Intestine
- Large Intestine
- Rectum and Anus
- Liver
- Gallbladder and Bile Ducts
- Pancreas
- Eating and Digestive Conditions
How Do We Fix it or Make it Better?
References, Attributions, and Image Descriptions
Digestive System: General Terms
| Term | Word Breakdown | Description |
|---|---|---|
| abdominal ab-dAH-muhn-l |
Suffix: -al pertaining to Combining form: |
Pertaining to the abdomen. The abdomen contains many vital organs: the stomach, the small intestine (jejunum and ileum), the large intestine (colon), the liver, the spleen, the gallbladder, the pancreas, the uterus, the fallopian tubes, the ovaries, the kidneys, the ureters, the bladder, and many blood vessels |
| gastrointestinal (GI) gas-troh-in-tEs-tuhn-l |
Suffix -al pertaining to Combing form: Combing form: |
Refers to the stomach and the intestines. However, the gastrointestinal track refers to the digestive system that leads from the mouth to the anus. |
Know the Basics!
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Digestive System.
Introduction to the Digestive System
The digestive system is continually at work, yet people seldom appreciate the complex tasks it performs in a choreographed biologic symphony. Consider what happens when you eat an apple. Of course, you enjoy the apple’s taste as you chew it, but in the hours that follow, unless something goes amiss and you get a stomachache, you don’t notice that your digestive system is working. You may be taking a walk or studying or sleeping, having forgotten all about the apple, but your stomach and intestines are busy digesting it and absorbing its vitamins and other nutrients. By the time any waste material is excreted, the body has appropriated all it can use from the apple. In short, whether you pay attention or not, the organs of the digestive system perform their specific functions, allowing you to use the food you eat to keep you going.
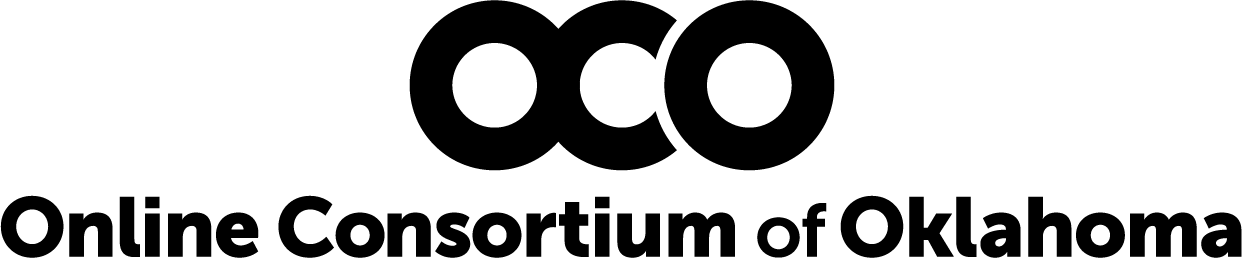
This chapter examines the structure and functions of these organs, and explores the mechanics and chemistry of the digestive processes. The function of the digestive system is to break down the foods you eat, release their nutrients, and absorb those nutrients into the body. Although the small intestine is the workhorse of the system, where the majority of digestion occurs, and where most of the released nutrients are absorbed into the blood or lymph, each of the digestive system organs makes a vital contribution to this process (see Figure 15.1).
Watch this video:
How Your Digestive System Works. Copyright 2018 by TED-Ed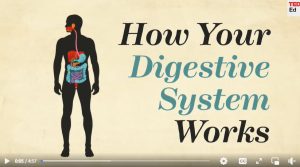
Digestive System Medical Terms
Now that you have memorized the word parts see if you can break down the following Digestive terms and define them.
Practice with this activity:
Anatomy (Structures) of the Digestive System
The Mouth
also called the oral cavity (or buccal cavity). The structures of the mouth are illustrated in Figure 15.2.
At the entrance to the mouth are the lips, or labia (singular = labium). Their outer covering is skin, which transitions to a mucous membrane in the mouth proper. Lips are very vascular with a thin layer of keratin; hence, the reason they are red.
The pocket-like part of the mouth that is framed on the inside by the gums and teeth, and on the outside by the cheeks and lips is called the oral vestibule. Moving farther into the mouth, the opening between the oral cavity and throat (oropharynx) is called the fauces (like the kitchen “faucet”). The main open area of the mouth, or oral cavity proper, runs from the gums and teeth to the fauces.
When you are chewing, you do not find it difficult to breathe simultaneously. The next time you have food in your mouth, notice how the arched shape of the roof of your mouth allows you to handle both digestion and respiration at the same time. This arch is called the palate. The anterior region of the palate serves as a wall (or septum) between the oral and nasal cavities as well as a rigid shelf against which the tongue can push food. It is created by the maxillary and palatine bones of the skull and, given its bony structure, is known as the hard palate. If you run your tongue along the roof of your mouth, you’ll notice that the hard palate ends in the posterior oral cavity, and the tissue becomes fleshier. This part of the palate, known as the soft palate, is composed mainly of skeletal muscle. You can therefore manipulate, subconsciously, the soft palate—for instance, to yawn, swallow, or sing (see Figure 15.2).
A fleshy bead of tissue called the uvula drops down from the center of the posterior edge of the soft palate. Although some have suggested that the uvula is a vestigial organ, it serves an important purpose. When you swallow, the soft palate and uvula move upward, helping to keep foods and liquid from entering the nasal cavity. Unfortunately, it can also contribute to the sound produced by snoring. Two muscular folds extend downward from the soft palate, on either side of the uvula. Toward the front, the palatoglossal arch lies next to the base of the tongue; behind it, the palatopharyngeal arch forms the superior and lateral margins of the fauces. Between these two arches are the palatine tonsils, clusters of lymphoid tissue that protect the pharynx. The lingual tonsils are located at the base of the tongue.
Tongue
Perhaps you have heard it said that the tongue is the strongest muscle in the body. Those who stake this claim cite its strength proportionate to its size. Although it is difficult to quantify the relative strength of different muscles, it remains indisputable that the tongue is a workhorse, facilitating ingestion, mechanical digestion, chemical digestion (lingual lipase), sensation (of taste, texture, and temperature of food), swallowing, and vocalization.
The tongue is attached to the mandible, the styloid processes of the temporal bones, and the hyoid bone. The hyoid is unique in that it only distantly/indirectly articulates with other bones. The tongue is positioned over the floor of the oral cavity. A medial septum extends the entire length of the tongue, dividing it into symmetrical halves.
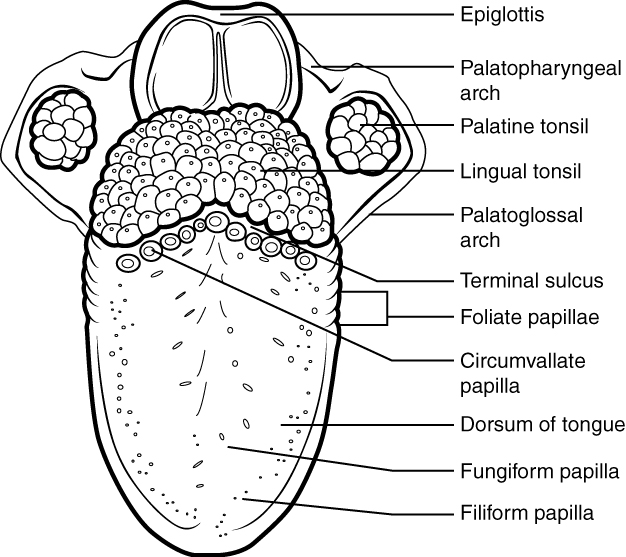
The top and sides of the tongue are studded with papillae, extensions of lamina propria of the mucosa, which are covered in stratified squamous epithelium (see Figure 15.3).
Salivary Glands
Many small salivary glands are housed within the mucous membranes of the mouth and tongue. These minor exocrine glands are constantly secreting saliva, either directly into the oral cavity or indirectly through ducts, even while you sleep. In fact, an average of 1 to 1.5 liters of saliva is secreted each day. Usually just enough saliva is present to moisten the mouth and teeth. Secretion increases when you eat, because saliva is essential to moisten food and initiate the chemical breakdown of carbohydrates. Small amounts of saliva are also secreted by the labial glands in the lips. In addition, the buccal glands in the cheeks, palatal glands in the palate, and lingual glands in the tongue help ensure that all areas of the mouth are supplied with adequate saliva.
Pharynx
The pharynx (throat) is involved in both digestion and respiration. It receives food and air from the mouth, and air from the nasal cavities. When food enters the pharynx, involuntary muscle contractions close off the air passageways. A short tube of skeletal muscle lined with a mucous membrane, the pharynx runs from the posterior oral and nasal cavities to the opening of the esophagus and larynx. It has three subdivisions. The most superior, the nasopharynx, is involved only in breathing and speech. The other two subdivisions, the oropharynx and the laryngopharynx, are used for both breathing and digestion. The oropharynx begins inferior to the nasopharynx and is continuous below with the laryngopharynx. The inferior border of the laryngopharynx connects to the esophagus, whereas the anterior portion connects to the larynx, allowing air to flow into the bronchial tree.
Esophagus
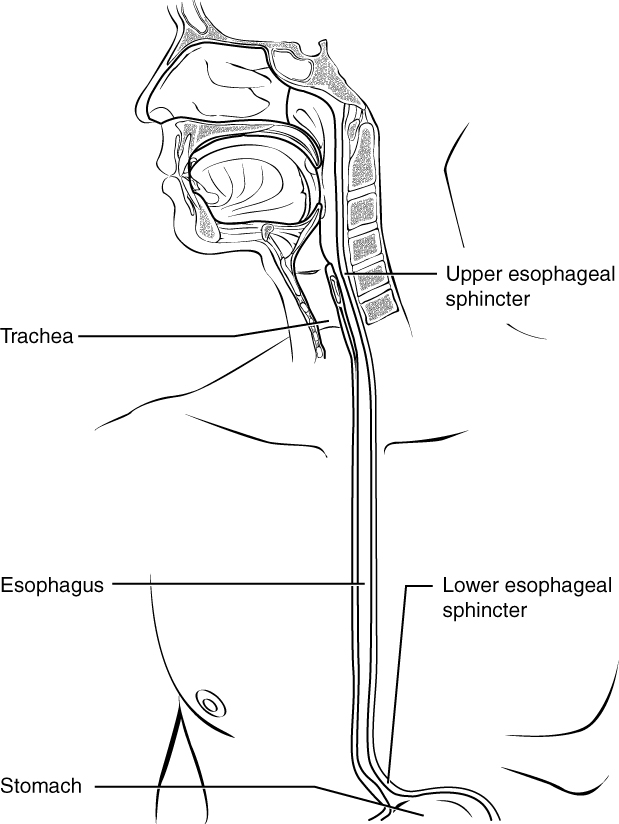
The esophagus is a muscular tube that connects the pharynx to the stomach. It is approximately 25.4 cm (10 in) in length, located posterior to the trachea, and remains in a collapsed form when not engaged in swallowing. As you can see in Figure 15.4, the esophagus runs a mainly straight route through the mediastinum of the thorax. To enter the abdomen, the esophagus penetrates the diaphragm through an opening called the esophageal hiatus.
Passage of Food Through the Esophagus
The upper esophageal sphincter, which is continuous with the inferior pharyngeal constrictor, controls the movement of food from the pharynx into the esophagus. The upper two-thirds of the esophagus consists of both smooth and skeletal muscle fibers, with the latter fading out in the bottom third of the esophagus. Rhythmic waves of peristalsis, which begin in the upper esophagus, propel the bolus of food toward the stomach. Meanwhile, secretions from the esophageal mucosa lubricate the esophagus and food. Food passes from the esophagus into the stomach at the lower esophageal sphincter (also called the gastroesophageal or cardiac sphincter). Recall that sphincters are muscles that surround tubes and serve as valves, closing the tube when the sphincters contract and opening it when they relax.
Stomach
There are four main regions in the stomach: the cardia, fundus, body, and pylorus (see Figure 15.5). The cardia (or cardiac region) is the point where the esophagus connects to the stomach and through which food passes into the stomach. Located inferior to the diaphragm, above and to the left of the cardia, is the dome-shaped fundus. Below the fundus is the body, the main part of the stomach. The funnel-shaped pylorus connects the stomach to the duodenum. The wider end of the funnel, the pyloric antrum, connects to the body of the stomach. The narrower end is called the pyloric canal, which connects to the duodenum. The smooth muscle pyloric sphincter is located at this latter point of connection and controls stomach emptying. In the absence of food, the stomach deflates inward, and its mucosa and submucosa fall into a large fold called a ruga.
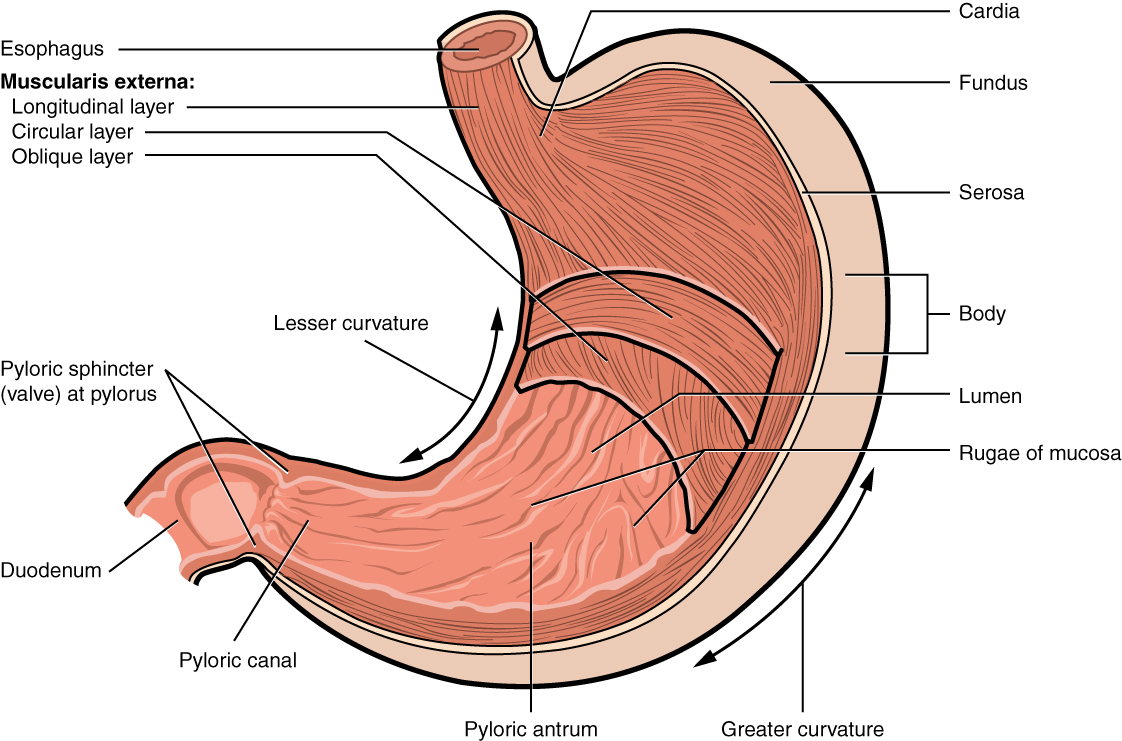
The convex lateral surface of the stomach is called the greater curvature; the concave medial border is the lesser curvature. The stomach is held in place by the lesser omentum, which extends from the liver to the lesser curvature, and the greater omentum, which runs from the greater curvature to the posterior abdominal wall.
Small Intestines
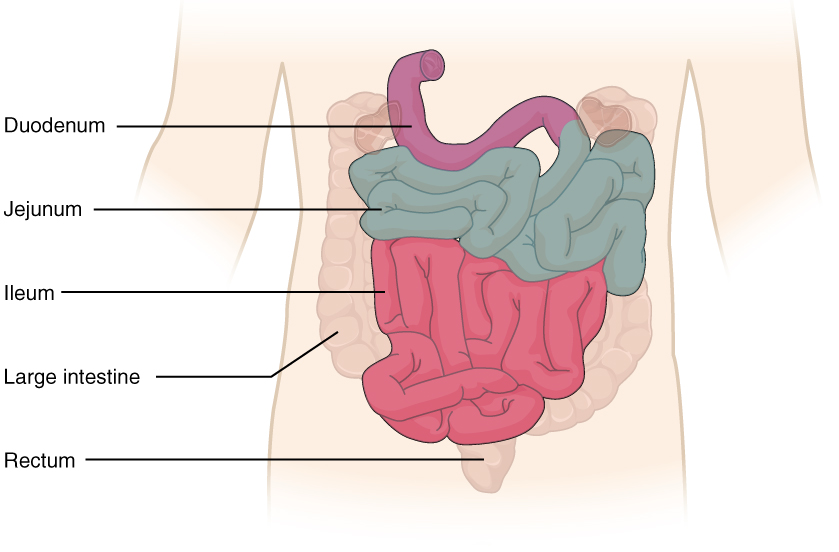
Chyme released from the stomach enters the small intestine, which is the primary digestive organ in the body. Not only is this where most digestion occurs, it is also where practically all absorption occurs. The longest part of the alimentary canal, the small intestine is about 3.05 meters (10 feet) long in a living person (but about twice as long in a cadaver due to the loss of muscle tone). Since this makes it about five times longer than the large intestine, you might wonder why it is called “small.” In fact, its name derives from its relatively smaller diameter of only about 2.54 cm (1 in), compared with 7.62 cm (3 in) for the large intestine. As we’ll see shortly, in addition to its length, the folds and projections of the lining of the small intestine work to give it an enormous surface area, which is approximately 200 m2, more than 100 times the surface area of your skin. This large surface area is necessary for complex processes of digestion and absorption that occur within it.
The coiled tube of the small intestine is subdivided into three regions. From proximal (at the stomach) to distal, these are the duodenum, jejunum, and ileum (see Figure 15.6).
Large Intestines
The large intestine is the terminal part of the alimentary canal. The primary function of this organ is to finish absorption of nutrients and water, synthesize certain vitamins, form feces, and eliminate feces from the body.
The large intestine runs from the appendix to the anus. It frames the small intestine on three sides. Despite its being about one-half as long as the small intestine, it is called large because it is more than twice the diameter of the small intestine, about 3 inches.
Cecum
The first part of the large intestine is the cecum, a sac-like structure that is suspended inferior to the ileocecal valve. It is about 6 cm (2.4 in) long, receives the contents of the ileum, and continues the absorption of water and salts. The appendix (or vermiform appendix) is a winding tube that attaches to the cecum. Although the 7.6-cm (3-in) long appendix contains lymphoid tissue, suggesting an immunologic function, this organ is generally considered vestigial. However, at least one recent report assumes a survival advantage conferred by the appendix: In diarrheal illness, the appendix may serve as a bacterial reservoir to repopulate the enteric bacteria for those surviving the initial phases of the illness. Moreover, its twisted anatomy provides a haven for the accumulation and multiplication of enteric bacteria. The mesoappendix, the mesentery of the appendix, tethers it to the mesentery of the ileum.
Colon
The cecum blends seamlessly with the colon. Upon entering the colon, the food residue first travels up the ascending colon on the right side of the abdomen. At the inferior surface of the liver, the colon bends to form the right colic flexure (hepatic flexure) and becomes the transverse colon. The region defined as hindgut begins with the last third of the transverse colon and continues on. Food residue passing through the transverse colon travels across to the left side of the abdomen, where the colon angles sharply immediately inferior to the spleen, at the left colic flexure (splenic flexure). From there, food residue passes through the descending colon, which runs down the left side of the posterior abdominal wall. After entering the pelvis inferiorly, it becomes the s-shaped sigmoid colon, which extends medially to the midline (see Figure 15.7). The ascending and descending colon, and the rectum (discussed next) are located in the retroperitoneum. The transverse and sigmoid colon are tethered to the posterior abdominal wall by the mesocolon.
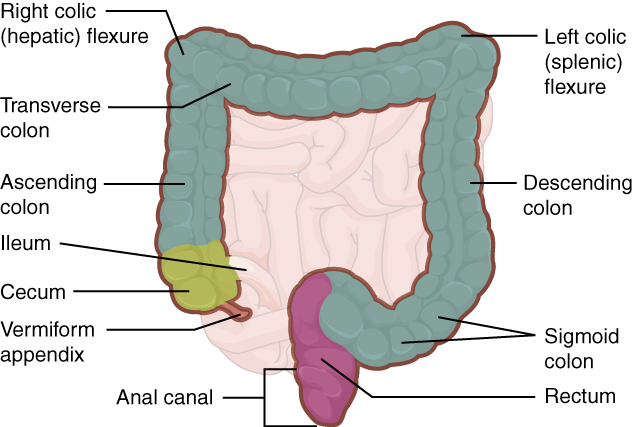
Figure 15.7 Large Intestine. The large intestine includes the cecum, colon, and rectum. From Betts, et al., 2013. Licensed under CC BY 4.0. [Image description.]
Accessory Organs of Digestion
Chemical digestion in the small intestine relies on the activities of three accessory digestive organs: the liver, pancreas, and gallbladder (see Figure 15.8). The digestive role of the liver is to produce bile and export it to the duodenum. The gallbladder primarily stores, concentrates, and releases bile. The pancreas produces pancreatic juice, which contains digestive enzymes and bicarbonate ions, and delivers it to the duodenum.
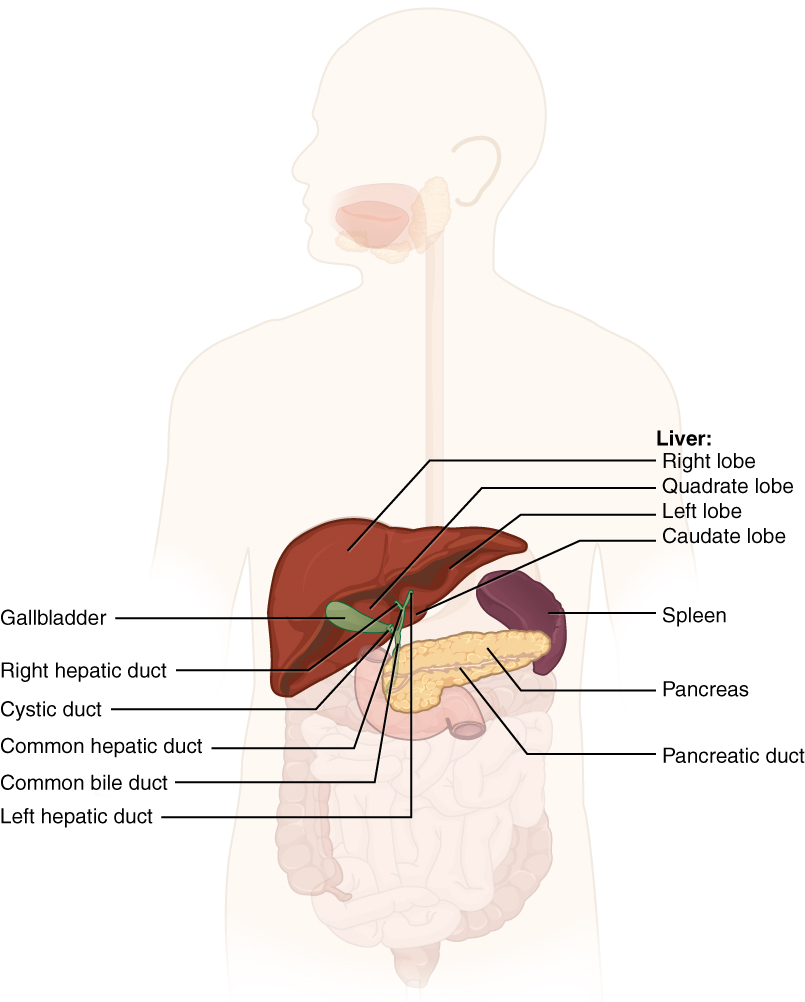
Liver
The liver is the largest gland in the body, weighing about three pounds in an adult. It is also one of the most important organs. In addition to being an accessory digestive organ, it plays a number of roles in metabolism and regulation. The liver lies inferior to the diaphragm in the right upper quadrant of the abdominal cavity and receives protection from the surrounding ribs.
The liver is divided into two primary lobes: a large right lobe and a much smaller left lobe. In the right lobe, some anatomists also identify an inferior quadrate lobe and a posterior caudate lobe, which are defined by internal features. The liver is connected to the abdominal wall and diaphragm by five peritoneal folds referred to as ligaments.
The porta hepatis (“gate to the liver”) is where the hepatic artery and hepatic portal vein enter the liver. These two vessels, along with the common hepatic duct, run behind the lateral border of the lesser omentum on the way to their destinations. The hepatic portal vein delivers partially deoxygenated blood containing nutrients absorbed from the small intestine and actually supplies more oxygen to the liver than do the much smaller hepatic arteries. In addition to nutrients, drugs and toxins are also absorbed. After processing the bloodborne nutrients and toxins, the liver releases nutrients needed by other cells back into the blood, which drains into the central vein and then through the hepatic vein to the inferior vena cava. With this hepatic portal circulation, all blood from the alimentary canal passes through the liver. This largely explains why the liver is the most common site for the metastasis of cancers that originate in the alimentary canal.
Bile produced by the liver is a mixture secreted by the liver to accomplish the emulsification of lipids in the small intestine.
Bilirubin, the main bile pigment, is a waste product produced when the spleen removes old or damaged red blood cells from the circulation. These breakdown products, including proteins, iron, and toxic bilirubin, are transported to the liver via the splenic vein of the hepatic portal system. In the liver, proteins and iron are recycled, whereas bilirubin is excreted in the bile. It accounts for the green color of bile. Bilirubin is eventually transformed by intestinal bacteria into stercobilin, a brown pigment that gives your stool its characteristic color! In some disease states, bile does not enter the intestine, resulting in white (‘acholic’) stool with a high fat content, since virtually no fats are broken down or absorbed.
Between meals, bile is produced but conserved. The valve-like hepatopancreatic ampulla closes, allowing bile to divert to the gallbladder, where it is concentrated and stored until the next meal.
Pancreas
The soft, oblong, glandular pancreas lies transversely in the retroperitoneum behind the stomach. Its head is nestled into the “c-shaped” curvature of the duodenum with the body extending to the left about 15.2 cm (6 in) and ending as a tapering tail in the hilum of the spleen. It is a curious mix of exocrine (secreting digestive enzymes) and endocrine (releasing hormones into the blood) functions (Figure 15.9).
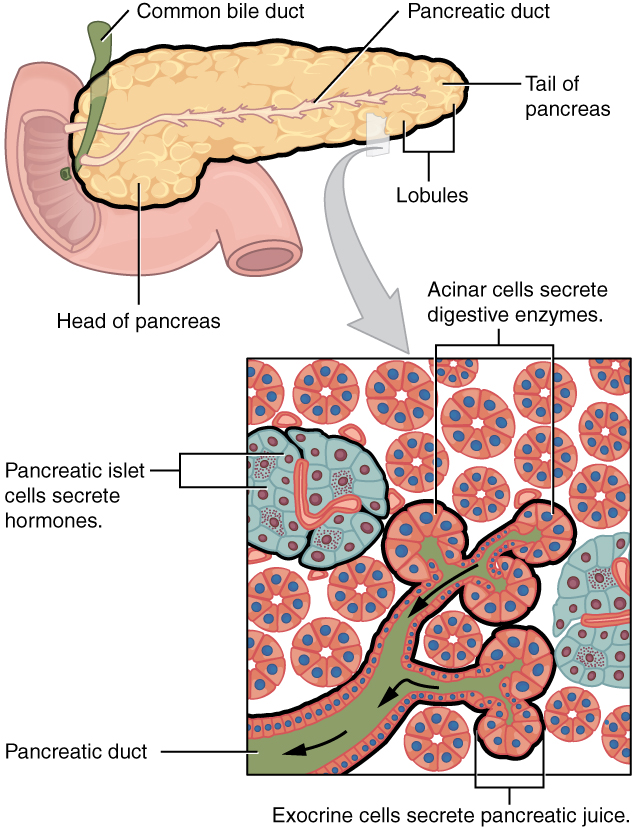
The exocrine part of the pancreas arises as little grape-like cell clusters, each called an acinus (plural = acini), located at the terminal ends of pancreatic ducts. These acinar cells secrete enzyme-rich pancreatic juice into tiny merging ducts that form two dominant ducts. The larger duct fuses with the common bile duct (carrying bile from the liver and gallbladder) just before entering the duodenum via a common opening (the hepatopancreatic ampulla). The smooth muscle sphincter of the hepatopancreatic ampulla controls the release of pancreatic juice and bile into the small intestine. The second and smaller pancreatic duct, the accessory duct (duct of Santorini), runs from the pancreas directly into the duodenum, approximately 1 inch above the hepatopancreatic ampulla. When present, it is a persistent remnant of pancreatic development.
Scattered through the sea of exocrine acini are small islands of endocrine cells, the islets of Langerhans. These vital cells produce the hormones pancreatic polypeptide, insulin, glucagon, and somatostatin.
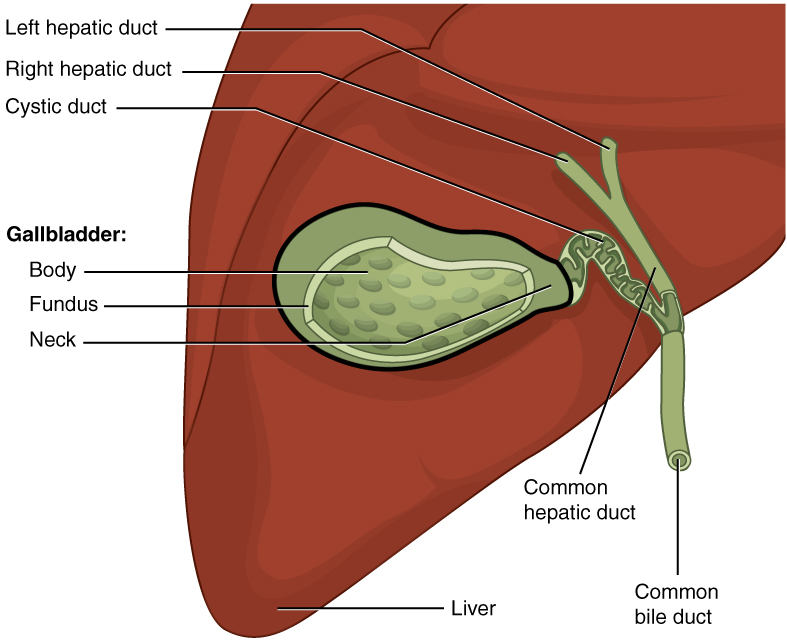
Gallbladder
The gallbladder is 8–10 cm (~3–4 in) long and is nested in a shallow area on the posterior aspect of the right lobe of the liver. This muscular sac stores, concentrates, and, when stimulated, propels the bile into the duodenum via the common bile duct. It is divided into three regions. The fundus is the widest portion and tapers medially into the body, which in turn narrows to become the neck. The neck angles slightly superiorly as it approaches the hepatic duct. The cystic duct is 1–2 cm (less than 1 in) long and turns inferiorly as it bridges the neck and hepatic duct.
The simple columnar epithelium of the gallbladder mucosa is organized in rugae, similar to those of the stomach. There is no submucosa in the gallbladder wall. The wall’s middle, muscular coat is made of smooth muscle fibers. When these fibers contract, the gallbladder’s contents are ejected through the cystic duct and into the bile duct (Figure 15.10). Visceral peritoneum reflected from the liver capsule holds the gallbladder against the liver and forms the outer coat of the gallbladder. The gallbladder’s mucosa absorbs water and ions from bile, concentrating it by up to 10-fold (Betts, et al., 2013).
Concept check
- Locate the cystic duct on the diagram shown.
- Consider what complications could arise if this duct was blocked or obstructed.
Watch this video:
Anatomy Labeling Activity
Physiology (Function) of the Digestive System
The main functions of the digestive system are:
- Ingesting food
- Digesting food
- Absorbing nutrients
- Elimination of waste products
Digestive Processes
The processes of digestion include six activities: ingestion, propulsion, mechanical or physical digestion, chemical digestion, absorption, and defecation.
The first of these processes, ingestion, refers to the entry of food into the alimentary canal through the mouth. There, the food is chewed and mixed with saliva, which contains enzymes that begin breaking down the carbohydrates in the food plus some lipid digestion via lingual lipase. Chewing increases the surface area of the food and allows an appropriately sized bolus to be produced.
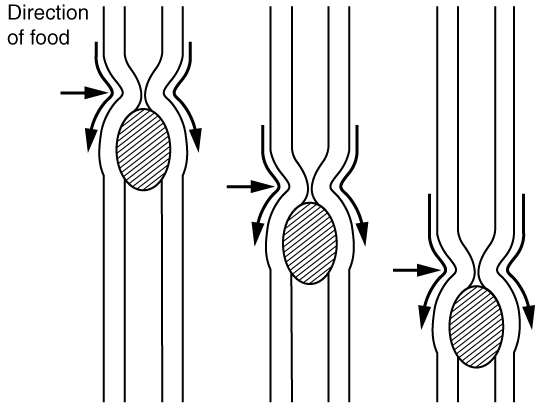
Food leaves the mouth when the tongue and pharyngeal muscles propel it into the esophagus. This act of swallowing, the last voluntary act until defecation, is an example of propulsion, which refers to the movement of food through the digestive tract. It includes both the voluntary process of swallowing and the involuntary process of peristalsis. Peristalsis consists of sequential, alternating waves of contraction and relaxation of alimentary wall smooth muscles, which act to propel food along (see Figure 15.11). These waves also play a role in mixing food with digestive juices. Peristalsis is so powerful that foods and liquids you swallow enter your stomach even if you are standing on your head.
Digestion includes both mechanical and chemical processes. Mechanical digestion is a purely physical process that does not change the chemical nature of the food. Instead, it makes the food smaller to increase both surface area and mobility. It includes mastication, or chewing, as well as tongue movements that help break food into smaller bits and mix food with saliva. Although there may be a tendency to think that mechanical digestion is limited to the first steps of the digestive process, it occurs after the food leaves the mouth, as well. The mechanical churning of food in the stomach serves to further break it apart and expose more of its surface area to digestive juices, creating an acidic “soup” called chyme. Segmentation, which occurs mainly in the small intestine, consists of localized contractions of circular muscle of the muscularis layer of the alimentary canal. These contractions isolate small sections of the intestine, moving their contents back and forth while continuously subdividing, breaking up, and mixing the contents. By moving food back and forth in the intestinal lumen, segmentation mixes food with digestive juices and facilitates absorption.
In chemical digestion, starting in the mouth, digestive secretions break down complex food molecules into their chemical building blocks (for example, proteins into separate amino acids). These secretions vary in composition, but typically contain water, various enzymes, acids, and salts. The process is completed in the small intestine.
Food that has been broken down is of no value to the body unless it enters the bloodstream and its nutrients are put to work. This occurs through the process of absorption, which takes place primarily within the small intestine. There, most nutrients are absorbed from the lumen of the alimentary canal into the bloodstream through the epithelial cells that make up the mucosa. Lipids are absorbed into lacteals and are transported via the lymphatic vessels to the bloodstream.
In defecation, the final step in digestion, undigested materials are removed from the body as feces.
Digestive System: From Appetite Suppression to Constipation
Age-related changes in the digestive system begin in the mouth and can affect virtually every aspect of the digestive system. Taste buds become less sensitive, so food isn’t as appetizing as it once was. A slice of pizza is a challenge, not a treat, when you have lost teeth, your gums are diseased, and your salivary glands aren’t producing enough saliva. Swallowing can be difficult, and ingested food moves slowly through the alimentary canal because of reduced strength and tone of muscular tissue. Neurosensory feedback is also dampened, slowing the transmission of messages that stimulate the release of enzymes and hormones.
Pathologies that affect the digestive organs—such as hiatal hernia, gastritis, and peptic ulcer disease—can occur at greater frequencies as you age. Problems in the small intestine may include duodenal ulcers, maldigestion, and malabsorption. Problems in the large intestine include hemorrhoids, diverticular disease, and constipation. Conditions that affect the function of accessory organs—and their abilities to deliver pancreatic enzymes and bile to the small intestine—include jaundice, acute pancreatitis, cirrhosis, and gallstones.
In some cases, a single organ is in charge of a digestive process. For example, ingestion occurs only in the mouth and defecation only in the anus. However, most digestive processes involve the interaction of several organs and occur gradually as food moves through the alimentary canal (see Figure 15.12).
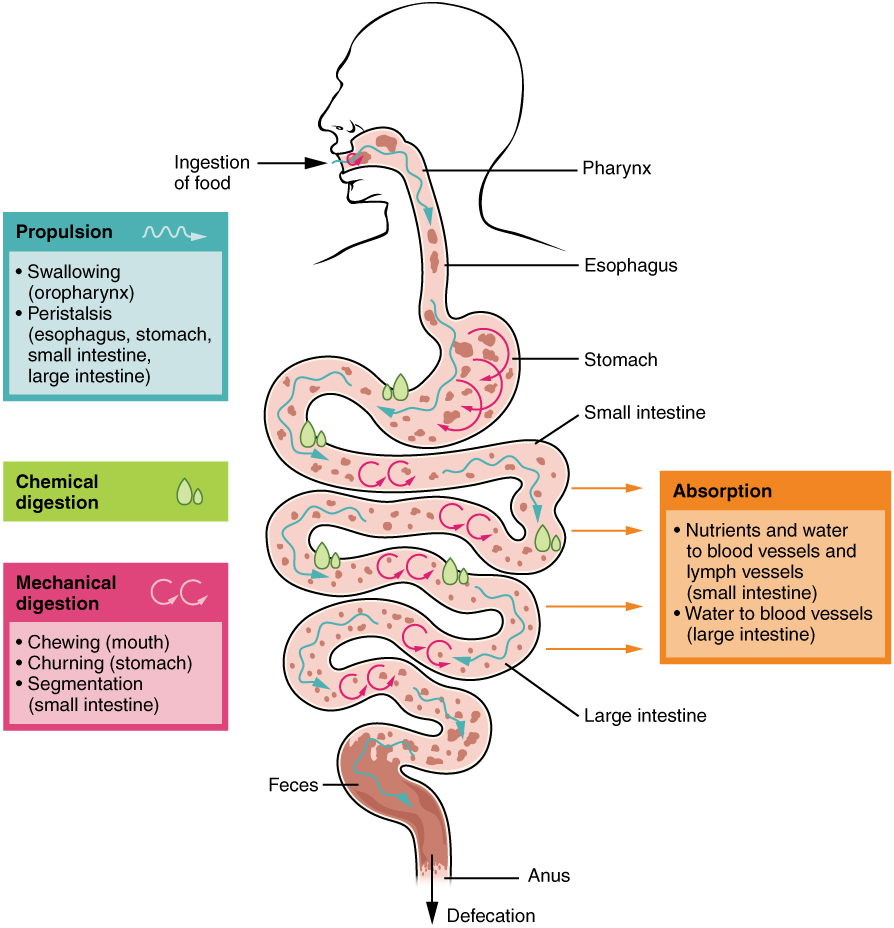
Some chemical digestion occurs in the mouth. Some absorption can occur in the mouth and stomach, for example, alcohol and aspirin.
Regulatory Mechanisms
Neural and endocrine regulatory mechanisms work to maintain the optimal conditions in the lumen needed for digestion and absorption. These regulatory mechanisms, which stimulate digestive activity through mechanical and chemical activity, are controlled both extrinsically and intrinsically.
Watch this video:
Media 15.2 Digestive System, Part 3: Crash Course A&P #35. Copyright 2015 by CrashCourse.
What Can Go Wrong? – Diseases, Disorders, and Conditions
Mouth, Lips Tongue, and Gum Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| cheilitis | -itis inflammation cheil/o |
Inflammation of the lip or lips |
| sialolithiasis | -iasis abnormal condition sial/o saliva, salivary gland lith/o |
Salivary stones, also called sialolithiasis, are hardened mineral deposits that form in the salivary glands. Read More |
| stomatitis stoh-muh-tIE-tuhs |
-itis inflammation stomat/o |
Inflammation of the mouth |
| gingivitis jin-juh-vIE-tuhs |
-itis inflammation gingiv/o |
Inflammation of the gums |
| glossitis glah-sIE-tuhs |
Suffix -itis inflammation Combing form: |
Inflammation of the tongue |
What Does that Mouth Do?
Esophagus, Stomach, and Abdominal Cavity Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| celiac disease sEE-lee-ak di-zEEz |
-ic pertaining to celi/o |
Celiac disease is an autoimmune disease where the ingestion of gluten leads to damage in the small intestine. Read more about celiac disease |
| dyspepsia dis-pEp-shuh |
-ia condition dys- peps/o |
Upset stomach |
| gastritis ga-strIE-tuhs |
-itis inflammation gastr/o
|
Inflammation of the stomach |
| gastroenteritis gas-troh-en-tuhr-rIE-tuhs |
-itis inflammation gastr/o enter/o |
Inflammation and irritation of the stomach and intestines. Read More about gastroenteritis |
| gastroesophageal reflux disease (GERD) gAs-troi-sah-fuh-jEE-uhl rEE-fluhks di-zEEz |
-al pertaining to gastr/o esophag/o |
Burning feeling in the chest (heart burn) that comes from acid made from the return of stomach contents up the esophagus and into the mouth. (regurgitation) . Video that explains GERD 1 min 59 seconds |
| hernia hUHR-nee-uh |
-ia condition herni/o |
When one of your organs pushes through the muscle or tissue that contains it. Often comes from heavy lifting. Read more about hernias |
| hyperemesis | -sis condition hyper emesis |
Excessive vomiting |
| peritonitis pair-uh-tuh-nIE-tuhs |
-itis inflammation peritone/o |
Inflammation of the peritoneum, the lining of the abdominal cavity |
| pyrosis pie-rOH-suhs |
-osis; usually abnormal condition pyr/o |
Heartburn |
Celiac Sprue (Celiac Disease)
Individuals who posses celiac disease have an immune sensitivity reaction occurring in the small intestines when they consume gluten. Typically people with this condition are genetically pre-disposed to the condition. Damage to the small intestine will occur if continued consumption of gluten occurs. Individuals once diagnosed eat a gluten free diet as a best approach for management of the condition. (Celiac Disease Foundation, n.d.). To learn more, visit the Celiac Disease Foundation’s What is Celiac Disease? article
Gastroesophageal Reflux Disease
This condition is largely caused by gastric acid flowing upwards from the stomach into the esophagus. Those suffering from the condition will often feel a burning sensation radiating near the top of the stomach. (Mayo Clinic Staff, 2020). To learn more about GERD visit the Mayo Clinic’s Gastroesophageal Reflux Disease (GERD) page.
Hernia
A hernia occurs when an organ or fatty tissue squeezes through a weak spot in a surrounding muscle or connective tissue. A hiatal hernia is found in the upper stomach region.
Digest This!
Small Intestine Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| ileus (il-ee-uh s) |
-us structure things ileum (the lower part of the small intestine) |
When your intestine stops making wave-like movements that push broken-down food and waste to to the anus and stimulate a bowel movement. Untreated ileus can lead to severe complications such as bowel perforation, infection, and sepsis. Read more about ileus |
| intussusception (in-tuh-suh-SEP-shun |
A condition in which part of the intestine slides into an adjacent part of the intestine. This telescoping action can block food or fluid from passing through. Intussusception also cuts off the blood supply to the part of the intestine that's affected. Read more about intussusception | |
| volvulus (vawl-yoo-luhs) |
-us structure things volv/o |
An obstruction (blockage) due to a knotting and twisting of part of the intestines |
Smaller Digest
Large Intestine Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| appendicitis uh-pen-duh-sIE-tuhs |
-itis inflammation append/o |
An inflammation of the appendix. The appendix is a finger-shaped pouch that sticks out from the colon on the lower right side of the belly, also called the abdomen. Read more about appendicitis |
| colitis koh-lIE-tuhs |
-itis inflammation
col/o |
Inflammation of the colon. It can cause abdominal pain, diarrhea, and rectal bleeding. Read More about colitis |
| diverticulum die-vuhr-tIk-yuh-luhm |
-um structure; tissue; thing diverticul/o- |
A single outpouching of the wall of the large intestine (colon) that forms a sac. |
| diverticula die-vuhr-tIk-yuh-luh |
diverticul/o- divertiulum |
Diverticula (plural)are multiple outpouching of the wall of the large intestine (colon) that forms a sac. |
| diverticulosis die-vuhr-tik-yuh-lOH-suhs |
-osis condition diverticul/o- |
Diverticulosis is the condition of having diverticulum or diverticula. Most people who have diverticulosis do not have symptoms or problems |
| diverticulitis die-vuhr-tik-yuh-lIE-tuhs |
-itis inflammation diverticul/o- |
When the diverticulum or diverticula become infected and inflamed. Infection can come from trapped feces. Video that describes diverticulitis, causes, signs and symptoms, Diagnosis and Treatment. |
| enteritis en-tuhr-rIE-tuhs |
-itis inflammation
enter/o |
Inflammation of the intestine |
| enteropathy en-tuhr-rAH-puh-thee |
-pathy disease enter/o |
Any disease of the intestine. |
| Irritable bowel syndrome (IBS) | A common, chronic, noninflammatory condition characterized by abdominal pain and altered bowel habits (diarrhea or constipation or both). There is no detectable pathologic change. Read more about IBS and watch a short video | |
| polyp pAH-luhp |
polyp/o polyp; small growth |
A small growth. A colorectal polyp refers to polyps in the colon and rectum. They are typically not dangerous but left untreated can become cancerous.
Video that explains polys and procedures to remove them (2 min 21 seconds) |
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a common disorder affecting the large intestines. IBS often involves abdominal pain as sensitive nerve tissue within the colon react to movement of food and waste through the digestive tract. Along with the abdominal pain individuals often experience gas and bloating. Diet and lifestyle modifications often help in the management of the condition. (Canadian Digestive Health Foundation, 2020b). To learn more about irritable bowel syndrome, visit the CDHF’s web page on IBS.
Polyps
A polyp is a small growth of tissue protruding outward from the intestinal wall. Some cancers in the intestines start off as a polyp. Typically, they are found in people over the age of 50. Polyps start as a small collection of cells found within the colon. Most are harmless but can transition over time into a cancerous growth (Mayo Clinic Staff, 2019). To learn more about polyps review the Mayo Clinic’s patient information page on polyps.
Larger Digest
Rectum and Anus Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| hemorrhoid (hEm-roidz) |
-oid resembling hem/o rrh/o |
Also called piles, are swollen varicose veins in the anus and lower rectum. Hemorrhoids can get irritated with the passing of feces. Read More |
| proctitis (prok-tahy-tis) |
-itis
proct/o |
Inflammation of the lining of the rectum. The rectum is a muscular tube that's connected to the end of your colon. Stool passes through the rectum on its way out of the body. Read More |
| rectocele (ret-rOH-seel) |
-cele
rect/o |
Rectoceles involve a herniation of the rectum into the vaginal wall that results in a vaginal bulge. Read more |
Rectum and Anus Conditions
Liver
| Term | Word Breakdown | Description |
|---|---|---|
| cirrhosis suhr-rOH-suhs |
-osis conditiohttps://open.ocolearnok.org/medicalterminology/wp-admin/admin.php?page=tablepressn |
A condition in which the liver is scarred and permanently damaged. Scar tissue replaces healthy liver tissue and prevents the liver from working normally. Scar tissue also partly blocks the flow of blood through the liver. As cirrhosis gets worse, the liver begins to fail Read more about cirrhosis |
| hepatitis hep-uh-tIE-tuhs |
-itis inflammation hepat/o |
Inflammation of the liver. Read more about hepatitis |
| hepatomegaly hep-uh-toh-mEg-uh-lee |
-megaly enlargement hepat/o |
Enlargement of the liver. Read more about hepatomegaly |
| hepatoma hep-uh-tOH-muh |
-oma tumor; mass; fluid collection hepat/o |
A tumor of the liver. The most common type of liver cancer. Hepatomas are almost always malignant. |
Cirrhosis
Cirrhosis is a condition whereby the liver scars. Advanced cirrhosis is life-threatening. It generally can not be reversed. It is caused by different forms of liver disease and chronic alcoholism. (Mayo Clinic Staff, 2018).
Cirrhosis often has no signs or symptoms until liver damage is extensive and may include:
-
-
- Fatigue
- Easily bleeding or bruising
- Loss of appetite
- Nausea
- Edema
- Weight loss
- Itchy skin
- Jaundice
- Ascitis (Mayo Clinic Staff, 2018)
-
To learn more about Cirrhosis visit the Mayo Clinic’s Cirrohsis web page .
Hepatitis A, B and C
Inflammation of the liver is referred to as hepatitis. This condition can be caused by several factors such as viruses, alcohol consumption, toxins, and drug interactions. In some cases, it can also be caused by an autoimmune response in the body. There are five types of viral hepatitis, A, B, C, D, and E (Booth, 2018). To learn more, visit Healthline’s article on Hepatitis.
Liver Conditions
Gallbladder and Bile Duct Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| cholangitis | Suffix: -itis inflammation Combining Form: Combining Form: |
inflammation of bile ducts Read more about cholangitis |
| cholecystitis (koh-luh-sis-tIE-tuhs) |
-itis inflammation cyst/o chol/e |
inflammation of the gallbladder Read more about cholecystitis |
| cholelithiasis (koh-luh-li-thIE-uh-suhs) |
-iasis condition; formation of chol/e lith/o |
the presence or formation of gallstones; Read more and watch a video about cholelithiasis |
Cholecystitis
This condition is known as inflammation of the gall bladder. Gallstone development can block the gall bladder’s release of bile leading to an inflammatory response. Surgical removal (cholecystectomy) or laser stone crushing known as lithotripsy are often the treatment options (“Cholecystitis”, 2019). To learn more about cholecystitis visit the Radiology Info’s cholecystitis web page.
The “Gall” of those “Ducts!”
Pancreas Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| pancreatitis pang-kree-uh-tIE-tuhs |
-itis inflammation pancreat/o |
inflammation of the pancreas. The pancreas is a large gland behind the stomach and close to the first part of the small intestine. It secretes digestive juices into the small intestine through a tube called the pancreatic duct. The pancreas also releases the hormones insulin and glucagon into the bloodstream. It happens when digestive enzymes start digesting the pancreas itself. |
“Pan-Create” Conditions
Eating and Digestive Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| anorexia an-uhr-rEk-see-uh |
Suffix: -ia condition Prefix: |
Lack of appetite |
| constipation kahn-stuh-pAY-shuhn |
Infrequent or difficult bowel movements | |
| diarrhea die-uhr-rEE-uh |
Suffix: -rrhea flow; discharge dia- across; through |
Abnormal frequency and liquidity of fecal discharges. |
| dysphagia dis-fAY-juh |
Suffix: -ia condition Prefix: Combining form: |
Difficulty in swallowing |
| flatulence flAch-uh-luhns |
Presence of excessive amounts of air or gas in the stomach or intestine, leading to distention (bloating) of the organs. | |
| hematochezia | Suffix: -ia condition Combining form: Combining form: |
Presence of blood in the feces. Read more about obstipation |
| obstipation | A severe form of constipation, where a person cannot pass stool or gas. Read more about obstipation | |
| polyphagia pah-lee-fAY-juh |
Suffix: -ia condition Prefix: Combining form: |
Excessive eating or hunger |
Digest these Conditions!
Laboratory and Diagnostic Procedures
| Term | Word Breakdown | Description |
|---|---|---|
| abdominocentesis ab-dAH-muhn-oh-sen-tEE-suhs |
-centesis surgical puncture to remove fluid abdomin/o |
A medical procedure where a needle is inserted into the abdominal cavity to remove fluid for diagnostic or therapeutic purposes. |
| cholangiography kuh-lan-jee-AH-gruh-fee |
-graphy
chol/e Combining form: |
Cholangiography means looking at the structure of the bile ducts and gallbladder using contrast materials. |
| colonoscopy koh-luh-nAH-skuh-pee |
-scopy the process of examining colon/o |
The insertion of a long, thin tube to examine the colon. The colon is the longest part of the large intestine. In addition to the colon, the large intestine include the rectum and anus. |
| endoscopy (en-dAH-skuh-pee) |
-scopy the process of examining endo- |
the insertion of a long, thin tube directly into the body to observe an internal organ — such as the gastrointestinal tract — in detail Video that shows a coloscopy a type of endoscopy |
| endoscope (En-duh-skohp) |
-scope
endo- |
The tool used in an endoscopy. A long thin tube with a camera attached |
| nasogastric tube – NG tube (nay-zoh-gAs-trik) |
-ic pertaining to nas/o gastr/o |
A nasogastric tube (NG tube) is a type of medical catheter that’s inserted through your nose into your stomach. It’s used for limited periods to deliver substances such as food or medications to your stomach or to draw substances out. Read more |
| upper gastrointestinal series (UGI) | -al pertaining to gastr/o intestin/o |
An upper GI series is a group of X-ray tests that look at your GI tract -- your food pipe (the esophagus), stomach, and the first part of your small intestine (the duodenum) while they're working. It's sometimes called UGI for short. Read more about UGI |
Upper and Lower Gastrointestinal Series
This is a diagnostic a procedure involving the introduction of a contrast medium known as barium. Barium can be introduced by ingesting or by enema. After induction of the barium, x-rays can be taken of the upper and lower gastrointestinal system structures (Johns Hopkins Medicine, 2020). To learn more, visit Johns Hopkins Medicine’s web page on barium x-rays.
Diagnostic Pop Quiz!
Surgical Procedures
| Term | Word Breakdown | Description |
|---|---|---|
| appendectomy ap-uhn-dEk-tuh-mee |
Suffix: -ectomy cut out; surgical removal Combing form:
|
Surgical removal of the appendix |
| cholecystectomy koh-luh-sis-tEk-tuh-mee |
Suffix: -ectomy cut out; surgical removal combining form: combining form: |
Surgical removal of the gall bladder |
| gastrectomy gAs-trEk-tuh-mee |
Suffix: -ectomy cut out; surgical removal combining form: |
surgical removal of all or part of the stomach. Read more about gastrectomy about gastrectomy |
| gastroplasty ga-str-OH-plas-tee |
Suffix: -plasty surgically rebuild combining form: |
a surgical procedure performed on the stomach to decrease its size or repair a defect |
| gastrostomy gAs-trAH-stuh-mee |
Suffix: -ostomy surgical creation of a new opening combining form: |
The surgical creation of a whole in the stomach that allows for tube feeding. |
| herniorrhaphy hUHR-nee-or-AH-fee |
Suffix: -tomy to suture |
Surgical repair of a hernia |
| laparotomy lap-uhr-rAH-tuh-mee |
Suffix: -tomy to cut into combining form: lapar/o abdominal wall; abdomen |
a surgical incision into the abdominal cavity, for diagnosis or in preparation for surgery. |
| polypectomy pAH-luhp-Ek-tuh-mee |
Suffix: -ectomy cut out; surgical removal Combining form: |
Surgical removal of polyps. Video that explains polys and procedures to remove them (2 min 21 seconds) |
Know your Procedures!
Drug Categories and References
| Term | Word Breakdown | Description |
|---|---|---|
| antacid ant-As-uhd |
Prefix: anti- against |
Drugs that help to treat heartburn (indigestion). They work by neutralizing the stomach acid that causes heartburn |
| antibiotic an-tie-bie-AH-tik |
Suffix: -al pertaining to Prefix: Combining form |
Medicines that fight infections caused by bacteria |
| antiemetic an-tie-i-mEt-ik |
Suffix: -ic pertaining to Prefix: |
Drugs that prevent or treat nausea and vomiting. |
| sublingual suhb-lIng-gwuhl |
Suffix: -al pertaining to Prefix: Combining form |
Under the tongue. Sublingual medications are placed under the tongue until they dissolve |
Drugs – Who am I?
Careers
| Term | Word Breakdown | Description |
|---|---|---|
| gastroenterologist gas-troh-en-tuhr-rAH-luh-jist |
-ist specialist gastr/o log/o Combining form: |
A physician with dedicated training management of diseases of the gastrointestinal tract and liver.Read more |
Gastroenterology
This specialty is focused on the diagnosis and treatment of conditions afflicting the digestive system. Gastroenterology is a branch of internal medicine. A physician who specializes in this area is known as a gastroenterologist. (Canadian Medical Association, 2018). To learn more about gastroenterology visit the Canadian Medical Association’s Gastroenterology profile page (PDF File).
Medical Terms in Context
Digestive System – Medical Report
Common Digestive Abbreviations
Test Yourself
References
Booth, S. (2018, August 13). Everything you need to know about hepatitis A, B, C, D, E. Healthline. https://www.healthline.com/health-news/everything-you-need-to-know-about-hepatitis#1
Canadian Medical Association. (2018, August). Gastroenterology profile. CMA Specialty Profiles. https://www.cma.ca/sites/default/files/2019-01/gastronenterology-e.pdf
Canadian Digestive Health Foundation. (2020). Esophageal cancer. https://cdhf.ca/digestive-disorders/esopagheal-cancer/what-is-esophageal-cancer/
Canadian Digestive Health Foundation. (2020a). Colon cancer. https://cdhf.ca/digestive-disorders/colon-cancer/
Canadian Digestive Health Foundation. (2020b). Irritable bowel syndrome. https://cdhf.ca/digestive-disorders/irritable-bowel-syndrome-ibs/
Celiac Disease Foundation. (n.d.) What is celiac disease?. Available from: https://celiac.org
“Cholecystitis”. (2019, January 15). Radiologyinfo.org. https://www.radiologyinfo.org/en/info.cfm?pg=cholecystitis
Crohns and Colitis Canada. (n.d.). What are Chron’s and colitis? https://crohnsandcolitis.ca/About-Crohn-s-Colitis/What-are-Crohns-and-Colitis
Johns Hopkins Medicine. (2020). Barium x-rays (upper and lower GI). https://www.hopkinsmedicine.org/health/conditions-and-diseases/barium-xrays-upper-and-lower-gi
Johns Hopkins Medicine. (2020a). Digestive diagnostic procedures. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/digestive-diagnostic-procedures
Mayo Clinic Staff. (2020, May 22). Gastroesophageal reflux disease. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940
Mayo Clinic Staff. (2018, December 7). Cirrhosis. Mayo Clinic. Available from: https://www.mayoclinic.org/diseases-conditions/cirrhosis/symptoms-causes/syc-20351487
Mayo Clinic Staff. (2019, October 19). Colon polyps. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/colon-polyps/symptoms-causes/syc-20352875
Attributions
Yeng Lor, intern at Tulsa Community College, fall 2023 contributed to the interactive activities in this chapter.
Image Descriptions
Figure 15.1 image description: This diagram shows the digestive system of a human being, with the major organs labeled. Labels read (clockwise, from top): salivary glands: parotid gland, sublingual gland, submandibular gland; pharynx, stomach, spleen, pancreas, large intestine: transverse colon, ascending colon, descending colon, cecum, sigmoid colon, appendix, rectum, anal canal, anus; small intestine: duodenum, jejunum, iliem, gall bladder, liver, esophagus, tongue, mouth. [Return to Figure 15.1].
Figure 15.2 image description: This diagram shows an anterior view of the structure of the mouth. The teeth, lips, tongue, gums and many other parts are labeled. Labels read (clockwise from top): superior lip, superior labial frenulum, gingivae, palatoglossal arch, fauces, palatopharyngeal arch, palatine tonsil, tongue, lingual frenulum, opening duct of submandibular gland, gingivae, inferior labial frenulum, inferior lip, oral vestibule, incisors, cuspid, premolars, molars, cheek, uvula, soft palate, hard palate. [Return to Figure 15.2].
Figure 15.3 image description: This diagram shows the structures of the tongue and lingual papillae. Labels read (from top): epiglottis, palatopharyngeal arch, palatine tonsil, lingual tonsil, palatoglossal arch, terminal sulcus, foliate papillae, circumvallate papilla, dorsum of tongue, fungiform papilla, filiform papilla. [Return to Figure 15.3].
Figure 15.4 image description: This diagram shows the esophagus, going from the mouth to the stomach. The upper and the lower esophageal sphincter are labeled. Labels read (from top): upper esophageal sphincter, trachea, esophagus, lower esophageal sphincter, stomach. [Return to Figure 15.4].
Figure 15.5 image description: This image shows a cross-section of the stomach, and the major parts: the cardia, fundus, body and pylorus are labeled. Labels read (from top of stomach): esophagus, muscular externa (longitudinal layer, circular layer, oblique layer), cardia, fundus, serosa, lesser and greater curvatures, lumen, rugae of mucosa, pyloric antrum, pyloric canal, pyloric sphincter valve at pylorus, duodenum. [Return to Figure 15.5].
Figure 15.6 image description: This diagram shows the small intestine. The different parts of the small intestine are labeled. Labels read (from top of small intestine): duodenum, jejunum, ilieum, large intestine, rectum. [Return to Figure 15.6].
Figure 15.7 image description: This image shows the large intestine; the major parts of the large intestine are labeled. Labels read (from start of large intestinal tract): vermiform complex, cecum, ileum, ascending colon, transverse colon, right colic hepatic flexure, left colic splenic flexure, descending colon, sigmoid colon, rectum, anal canal. [Return to Figure 15.7].
Figure 15.8 image description: This diagram shows the accessory organs of the digestive system. The liver, spleen, pancreas, gallbladder and their major parts are shown. Labels read: liver (right lobe, quadrate lobe, left lobe, caudate lobe), spleen, pancreas, pancreatic duct, gall bladder right hepatic duct, cystic duct, common hepatic duct, common bile duct, left hepatic duct. [Return to Figure 15.8].
Figure 15.9 image description: This figure shows the pancreas and its major parts Labels read (from left to right): common bile duct, head of pancreas, pancreatic duct, lobules, tail of pancreas. A magnified view of a small region of the pancreas shows the pancreatic islet cells, the acinar cells, exocrine cells, and the pancreatic duct. [Return to Figure 15.9].
Figure 15.10 image description: This figure shows the gallbladder and its major parts are labeled. Labels read (starting in gallbladder): body, fundus, neck, cystic duct, common hepatic duct, common bile duct, left and right hepatic ducts, liver. [Return to Figure 15.10].
Figure 15.11 image description: This image shows the peristaltic movement of food. In the left image, the food bolus is towards the top of the esophagus and arrows pointing downward show the direction of movement of the peristaltic wave. In the center image, the food bolus and the wave movement are closer to the center of the esophagus and in the right image, the bolus and the wave are close to the bottom end of the esophagus. [Return to Figure 15.11].
Figure 15.12 image description: This image shows the different processes involved in digestion. The image shows how food travels from the mouth through the major organs. Associated textboxes list the various digestive processes: Absorption (nutrients and water to blood vessels and lymph vessels (small intestine), water to blood vessels (large intestine)), propulsion (swallowing (oropharynx), peristalsis (esophagus, stomach, small intestine, large intestine), chemical digestion, mechanical digestion (chewing (mouth), churning (stomach), segmentation (small intestine)). Parts of the digestive tract are labelled: ingestion of food, pharynx, esophagus, stomach, small intestine, large intestine, feces, anus, defecation. [Return to Figure 15.12].
Unless otherwise indicated, this chapter
contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
lips of the mouth
The inside of your nose.
a pair of soft tissue masses located at the rear of the throat (pharynx)
collection of lymphatic tissue located in the lamina propria of the root of the tongue
Cells arranged in layers upon a basal membrane
to secrete externally, directly or through a duct
The sugars, starches and fibers found in fruits, grains, vegetables and milk products.
A band of smooth muscle at the junction between the pylorus of the stomach and the duodenum of the small intestine
Curved outwards
Fatty tissue that stretches over the abdomen, plays a role in immune response and the growth of certain cancers
situated nearer to the center of the body or the point of attachment
Away from the center of the body or from the point of attachment
Resembling lymph or lymphatic tissues
A by-product of the body's metabolism
A square or rectangular.
The process of breaking down the fat into smaller blood cells which makes it easy for enzymes to function and digest food.
A concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs
A sac-like enlargement of a canal or duct
A part of a hollow organ
The lymphatic vessels of the small intestine which absorb digested fats
Relating to afferent nerves
Location where the diaphragm has a small opening (hiatus) through which the esophagus passes before connecting.
Poor breakdown of food
A disorder that occurs when people are unable to absorb nutrients from their diets