8 Blood, Lymphatic and Immune Systems
Learning Objectives
- Identify general terms related to the blood, lymphatics, and immune systems.
- Spell the blood, lymphatics, and immune system medical terms and use the correct abbreviations
- Identify the medical specialties associated with the blood, lymphatics, and immune systems.
- Recognize common diseases, disorders, and procedures related to the blood, lymphatics, and immune systems.
Chapter Eight: Table of Contents
What is it?
What Can Go Wrong? – Diseases, Disorders, and Conditions of the Blood, Lymphatic, and Immune Systems
- General Blood
- Erythrocytes (Red Blood Cells)
- Leukocytes (White blood cells)
- Thrombocytes (Platelets)
- Plasma
- Lymphatic System
How Do We Fix it or Make it Better?
References, Attributions, and Image Descriptions
Blood
| Term | Word Breakdown | Description |
|---|---|---|
| coagulation koh-ag-yuh-lAY-shuhn |
-ation process; condition coagul/o
|
The process of becoming viscous or thickened into a coherent mass : the forming of clots |
| electrolyte i-lEk-truh-liet |
Minerals (such as include sodium, calcium, and potassium) in your blood and other body fluids that carry an electric charge. Electrolytes affect how your body functions in many ways, including: The amount of water in your body. The acidity of your blood (pH) and your muscle function. | |
| erythrocyte i-rIth-ruh-siet |
-cyte cell erythr/o |
Red blood cell |
| hematology hee-muh-tAH-luh-jee |
-logy study of hemat/o |
A medical science that deals with the blood |
| hemopoiesis hee-muh-poi-EE-suhs |
-poiesis formation hem/o |
The formation of blood or of blood cells (white blood cells, red blood cells, and platelets). |
| hemostasis hee-muh-stAY-suhs |
-stasis level; unchanging hem/o |
The stopping of bleeding |
| homeostasis hoh-mee-oh-stAY-suhs |
-stasis level; unchanging home/o |
Maintaining a constant internal environment.
Video explanation Video explanation |
| leukocyte lOO-kuh-siet |
-cyte cell leuk/o |
A white blood cell. It plays an essential role in defending the body against infection. |
| megakaryocyte meg-uh-kAr-ee-oh-siet |
-cyte cell mega- |
A large cell responsible for the everyday production and release of platelets into the bloodstream. |
| phagocyte fAg-uh-siet |
-cyte cell phag/o |
A cell (such as a macrophage or neutrophil) that engulfs and consumes foreign material (such as microorganisms) and debris (such as dead tissue cells) |
| plasma plAz-muh |
The fluid part of blood. Plasma is responsible for:
Redistributing water where your body needs it. |
|
| thrombocyte thrAHm-buh-siet |
-cyte cell thromb/o |
Platelet; a cell with clotting functions |
| thrombus thrAHm-bie |
-osis condition thromb/o |
A clot of blood formed within a blood vessel and remaining attached to its place of origin. A thrombi is the plural form of thrombus and refers to multiple clots. |
Blood and Blood Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Cardiovascular System - Blood.
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Lymphatic and Immune Systems.
The Composition (Anatomy) of Blood and the Functions of the Components
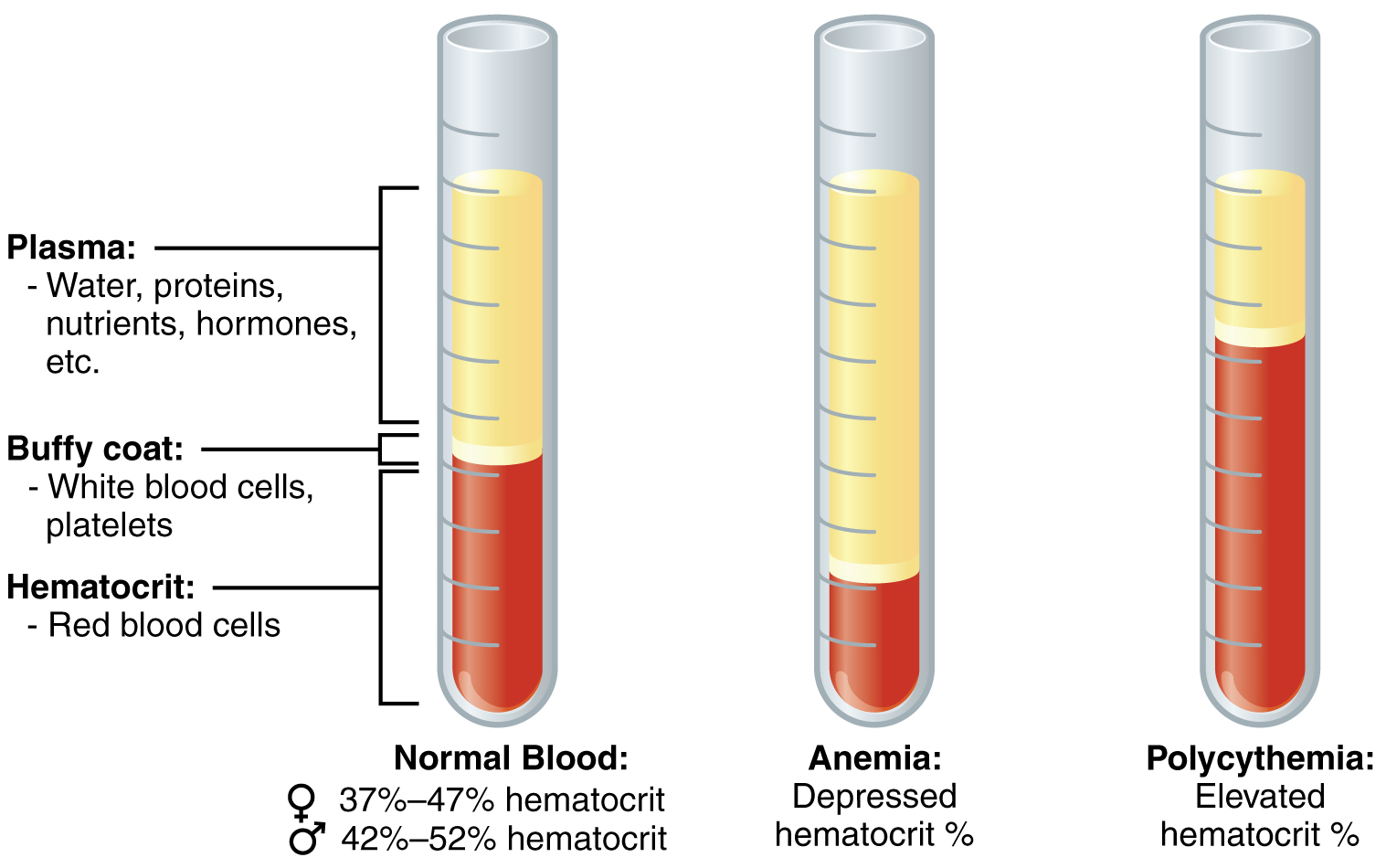
In the laboratory, blood samples are often centrifuged in order to separate the components of blood from one another (see the figure below). Erythrocytes are the heaviest elements in blood and settle at the very bottom of the tube. Above the erythrocyte layer we see the buffy coat, a pale, thin layer of leukocytes and thrombocytes, which together make up less than 1% of the sample of whole blood. Above the buffy coat is the blood plasma, normally a pale, straw-colored fluid, which constitutes the remainder of the sample.
In normal blood, about 45 percent of a sample is erythrocytes, which is referred to as the hematocrit. The hematocrit of any one sample can vary significantly, however, about 36–50 percent, according to gender and other factors. Not counting the buffy coat, which makes up less than 1% of the blood, we can estimate the mean plasma percentage to be the percent of blood that is not erythrocytes: approximately 55%.
Blood Plasma
Like other fluids in the body, plasma is composed primarily of water. In fact, it is about 92% water. Dissolved or suspended within this water is a mixture of substances, most of which are proteins. The major components of plasma and their functions are summarized in the table above.
Formed Elements (Erythrocytes, Leukocytes, Thrombocytes) Add link to supplemental document
Hemopoiesis/Hematopoiesis
The lifespan of the formed elements is very brief. Although one type of leukocyte (memory cells) can survive for years, most erythrocytes, leukocytes, and platelets normally live only a few hours to a few weeks. Thus, the body must form new blood cells and platelets quickly and continuously, a process known as hemopoiesis.
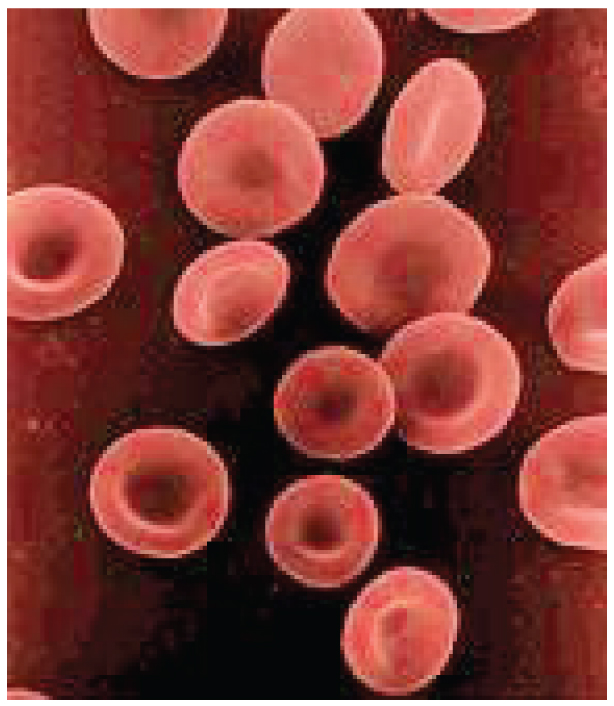
Erythrocytes
The most abundant formed elements in blood, erythrocytes are basically sacs packed with an oxygen-carrying compound called hemoglobin. Production of erythrocytes in the red bone marrow occurs at the staggering rate of more than 2 million cells per second. Erythrocytes live only 120 days on average, and thus must be continually replaced. Worn-out erythrocytes are phagocytized by macrophages and their hemoglobin is broken down. The breakdown products are recycled or removed as wastes.
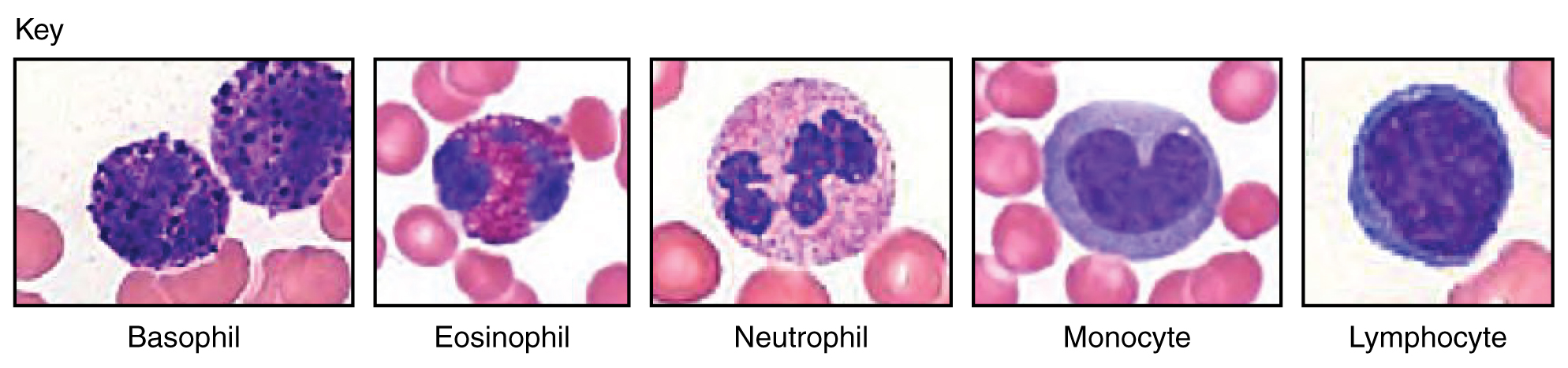
Leukocytes
Concept Check
- What is the function of an erythrocyte?
- What is the major function of the leukocytes?
Platelets
After entering the circulation, approximately one-third of the newly-formed platelets migrate to the spleen for storage for later release in response to any rupture in a blood vessel. They then become activated to perform their primary function, which is to limit blood loss. Platelets remain only about 10 days, then are phagocytized by macrophages.
Platelets are key players in hemostasis, the process by which the body seals a ruptured blood vessel and prevents further loss of blood. Although rupture of larger vessels usually requires medical intervention, hemostasis is quite effective in dealing with small, simple wounds. There are three steps to the process: vascular spasm, the formation of a platelet plug, and coagulation (blood clotting). Failure of any of these steps will result in hemorrhage. The figure below summarizes the steps of hemostatis.
Concept Check
- Can you explain what happens in each step of hemostasis?
- Describe an anticoagulant.
Physiology of Blood
Although carrying oxygen and nutrients to cells and removing wastes from cells is the main function of blood, it is important to realize that blood also serves in defense, distribution of heat, and maintenance of homeostasis.
Transportation
- Nutrients from the foods you eat are absorbed in the digestive tract. Most of these travel in the bloodstream directly to the liver, where they are processed and released back into the bloodstream for delivery to body cells.
- Oxygen from the air you breathe diffuses into the blood, which moves from the lungs to the heart, which then pumps it out to the rest of the body.
- Endocrine glands scattered throughout the body release their products, called hormones, into the bloodstream, which carries them to distant target cells.
- Blood also picks up cellular wastes and byproducts, and transports them to various organs for removal. For instance, blood moves carbon dioxide to the lungs for exhalation from the body, and various waste products are transported to the kidneys and liver for excretion from the body in the form of urine or bile.
Defense
- Leukocytes protect the organism from disease-causing bacteria, cells with mutated DNA that could multiply to become cancerous, or body cells infected with viruses.
- When damage to the vessels results in bleeding, blood platelets and certain proteins dissolved in the plasma, interact to block the ruptured areas of the blood vessels involved. This protects the body from further blood loss.
Homeostasis
- If you were exercising on a warm day, your rising core body temperature would trigger several homeostatic mechanisms, including increased transport of blood from your core to your body periphery, which is typically cooler. As blood passes through the vessels of the skin, heat would be dissipated to the environment, and the blood returning to your body core would be cooler. In contrast, on a cold day, blood is diverted away from the skin to maintain a warmer body core. In extreme cases, this may result in frostbite.
- Blood helps to regulate the water content of body cells.
- Blood also helps to maintain the chemical balance of the body. Proteins and other compounds in blood act as buffers, which thereby help to regulate the pH of body tissues. The pH of blood ranges from 7.35 to 7.45.
Concept Check
These three terms all sound similar. Can you explain them by breaking down the word parts?
- Hemostasis
- Homeostasis
- Hemopoiesis
Additional Information Blood Types and Hemolytic Disease of the Newborn (HDN)
Introduction to the Lymphatic and Immune Systems
| Term | Word Breakdown | Description |
|---|---|---|
| antigen An-tij-uhn |
-gen formation; producing anti- |
Any substance that evokes an immune response |
| antibody An-ti-bah-deez |
anti- against |
A protein produced by the immune system to neutralize pathogens |
| autoimmune aw-toim-yOOn |
immun/o Immunity; safe auto- |
A condition in which the immune system mistakenly attacks the body's own cells |
| endemic en-dEm-ik |
-ic pertaining to en- dem/o |
A disease or outbreak of disease that is typically present in a particular region or population : an endemic disease |
| epidemic ep-uh-dEm-ik |
-ic pertaining to epi- dem/o |
A disease that affects a disproportionately large number of individuals within a population, community, or region at the same time, |
| immunity i-myOO-nuh-tee |
immun/o Immunity; safe |
The ability of the body to resist infection and disease |
| pandemic pan-dEm-ik |
-ic pertaining to dem/o pan- |
An outbreak that occurs over a wide geographic area (such as multiple countries or continents) and typically affecting a significant proportion of the population |
| pathogen pAth-uh-juhn |
path/o disease -gen |
A microorganism that causes disease |
| macrophage mAk-ruh-fayj |
macro- large; long; big phag/o |
A type of white blood cell that engulfs and destroys pathogens |
The lymph system is a network of organs, lymph nodes, lymph ducts, and lymph vessels that make and move lymph from tissues to the bloodstream. The lymph system is a major part of the body's immune system.
Watch this video:
Components of the Lymphatic System
The lymphatic system consists of a fluid (lymph), vessels that transport the lymph, and organs that contain lymphoid tissue.
Lymph
Lymph is a fluid similar in composition to blood plasma. It is derived from blood plasma as fluids pass through capillary walls at the arterial end. As the interstitial fluid begins to accumulate, it is picked up and removed by tiny lymphatic vessels and returned to the blood. As soon as the interstitial fluid enters the lymph capillaries, it is called lymph. Returning the fluid to the blood prevents edema and helps to maintain normal blood volume and pressure.
Lymphatic Vessels
Lymphatic vessels, unlike blood vessels, only carry fluid away from the tissues. The smallest lymphatic vessels are the lymph capillaries, which begin in the tissue spaces as blind-ended sacs. Lymph capillaries are found in all regions of the body except the bone marrow, central nervous system, and tissues, such as the epidermis, that lack blood vessels. The wall of the lymph capillary is composed of endothelium in which the simple squamous cells overlap to form a simple one-way valve. This arrangement permits fluid to enter the capillary but prevents lymph from leaving the vessel.
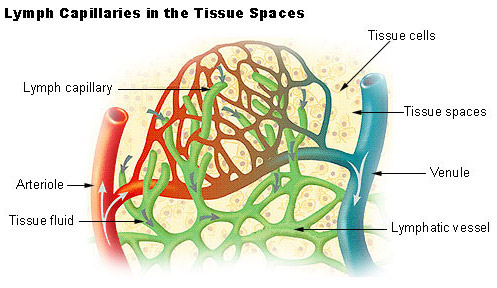
The microscopic lymph capillaries merge to form lymphatic vessels. Small lymphatic vessels join to form larger tributaries, called lymphatic trunks, which drain large regions. Lymphatic trunks merge until the lymph enters the two lymphatic ducts. The right lymphatic duct drains lymph from the upper right quadrant of the body. The thoracic duct drains all the rest.
Like veins, the lymphatic tributaries have thin walls and have valves to prevent backflow of blood. There is no pump in the lymphatic system like the heart in the cardiovascular system. The pressure gradients to move lymph through the vessels come from the skeletal muscle action, respiratory movement, and contraction of smooth muscle in vessel walls.
Lymphatic Organs
Lymphatic organs are characterized by clusters of lymphocytes and other cells, such as macrophages, enmeshed in a framework of short, branching connective tissue fibers. The lymphocytes originate in the red bone marrow with other types of blood cells and are carried in the blood from the bone marrow to the lymphatic organs. When the body is exposed to microorganisms and other foreign substances, the lymphocytes proliferate within the lymphatic organs and are sent in the blood to the site of the invasion. This is part of the immune response that attempts to destroy the invading agent.
The lymphatic organs include:
The Organization of the Immune System
Cells of the Innate Immune Response
Phagocytes: Macrophages and Neutrophils
A phagocyte is a cell that is able to surround and engulf a particle or cell, a process called phagocytosis. The phagocytes of the immune system engulf other particles or cells, either to clean an area of debris, old cells, or to kill pathogenic organisms such as bacteria. Macrophages, neutrophils, and dendritic cells are the major phagocytes of the immune system and are the body’s fast acting, front line immunological defense against organisms that have breached barrier defenses and have entered the body.
Macrophages not only participate in innate immune responses but have also evolved to cooperate with lymphocytes as part of the adaptive immune response. Macrophages exist in many tissues of the body, either freely roaming through connective tissues or fixed to reticular fibers within specific tissues such as lymph nodes. When pathogens breach the body’s barrier defenses, macrophages are the first line of defense.
A neutrophil is a phagocytic cell that is attracted via chemotaxis from the bloodstream to infected tissues. contains cytoplasmic granules, which in turn contain a variety of vasoactive mediators such as histamine. Whereas macrophages act like sentries, always on guard against infection, neutrophils can be thought of as military reinforcements that are called into a battle to hasten the destruction of the enemy.
A monocyte is a circulating precursor cell that differentiates into either a macrophage or dendritic cell, which can be rapidly attracted to areas of infection by signal molecules of inflammation.
Inflammatory Response
The hallmark of the innate immune response is inflammation. Stub a toe, cut a finger, or do any activity that causes tissue damage and inflammation will result, with its four characteristics: heat, redness, pain, and swelling (“loss of function” is sometimes mentioned as a fifth characteristic). It is important to note that inflammation does not have to be initiated by an infection, but can also be caused by tissue injuries. The release of damaged cellular contents into the site of injury is enough to stimulate the response, even in the absence of breaks in physical barriers that would allow pathogens to enter (by hitting your thumb with a hammer, for example). The inflammatory reaction brings in phagocytic cells to the damaged area to clear cellular debris and encourages the entry of clotting factors to set the stage for wound repair. Inflammation also facilitates the transport of antigen to lymph nodes by dendritic cells for the development of the adaptive immune response.
What Can Go Wrong? – Diseases, Disorders, and Conditions of the Blood, Lymphatic, and Immune Systems
General Diseases, Disorders or Conditions of the Blood
| Term | Word Breakdown | Description |
|---|---|---|
| dyscrasia dis-krAY-zhuh |
-ia condition dys- cras/o |
A nonspecific term that refers to a disease or disorder, especially of the blood. |
| hemorrhage hEm-uhr-rij |
-rrhage bleeding hem/o |
A heavy discharge of blood from the blood vessels |
| pancytopenia pan-sie-tuh-pEE-nee-uh |
-penia deficiency; lack of pan- cyt/o |
Low levels of all three blood cell types: red blood cells, white blood cells and platelets. |
| septicemia sep-tuh-sEE-mee-uh |
-emia blood condition seps/o |
A serious bloodstream infection.
It occurs when a bacterial infection enters the bloodstream from elsewhere in the body |
Hemorrhage
Minor blood loss is managed by hemostasis and repair. Hemorrhage is a loss of blood that cannot be controlled by hemostatic mechanisms. Initially, the body responds to hemorrhage by initiating mechanisms aimed at increasing blood pressure and maintaining blood flow. Ultimately, however, blood volume will need to be restored, either through physiological processes or through medical intervention. If blood loss is less than 20 percent of total blood volume, fast-acting homeostatic mechanisms causing increased cardiac output and vasoconstriction, would usually return blood pressure to normal and redirect the remaining blood to the tissues. Blood volume will then need to be restored via slower-acting homeostatic mechanisms, to increase body fluids and erythrocyte production (Betts, et al., 2013).
Circulatory Shock
The loss of too much blood may lead to circulatory shock, a life-threatening condition in which the circulatory system is unable to maintain blood flow to adequately supply sufficient oxygen and other nutrients to the tissues to maintain cellular metabolism. It should not be confused with emotional or psychological shock. Typically, the patient in circulatory shock will demonstrate an increased heart rate but decreased blood pressure. Urine output will fall dramatically, and the patient may appear confused or lose consciousness. Unfortunately, shock is an example of a positive-feedback loop that, if uncorrected, may lead to the death of the patient (Betts, et al., 2013).
There are several recognized forms of shock:
- Hypovolemic shock in adults is typically caused by hemorrhage, although in children it may be caused by fluid losses related to severe vomiting or diarrhea.
- Cardiogenic shock results from the inability of the heart to maintain cardiac output. Most often, it results from a myocardial infarction (heart attack), but it may also be caused by arrhythmias, valve disorders, cardiomyopathies, cardiac failure, or simply insufficient flow of blood through the cardiac vessels.
- Vascular shock occurs when arterioles lose their normal muscular tone and dilate dramatically. It may arise from a variety of causes, and treatments almost always involve fluid replacement and medications, called inotropic or pressor agents, which restore tone to the muscles of the vessels.
- Anaphylactic shock is a severe allergic response that causes the widespread release of histamines, triggering vasodilation throughout the body.
- Obstructive shock, as the name would suggest, occurs when a significant portion of the vascular system is blocked. It is not always recognized as a distinct condition and may be grouped with cardiogenic shock, including pulmonary embolism and cardiac tamponade. Treatments depend upon the underlying cause and, in addition to administering fluids intravenously, often include the administration of anticoagulants, removal of fluid from the pericardial cavity, or air from the thoracic cavity, and surgery as required. The most common cause is a pulmonary embolism. Other causes include stenosis of the aortic valve; cardiac tamponade; and a pneumothorax (Betts, et al., 2013).
Erythrocytes- Diseases Disorders or Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| anisocytosis | -osis condition; usually abnormal anis/o cyt/o |
Variation (unequal) size of cells and especially of the red blood cells. |
| anemia uh-nEE-mee-uh |
-emia blood condition an- |
A condition characterized by a decrease in the number of red blood cells or a decrease in the amount of hemoglobin in the blood |
| hemolytic ˌhiməˈlɪtɪk |
-lytic pertaining to break down, destruction; dissolving hem/o lyt/o |
Pertaining to the destruction of red blood cells |
| hypochromic hie-puh-krOH-mik |
-ic pertaining to hypo- chrom/o |
Abnormally pale red blood cells. Comes from red blood cells with deficient hemoglobin. |
| macrocytic mak-ruh-sIt-ik |
-ic pertaining to |
Pertaining to an exceptionally large red blood cell. |
| microcytic mie-kruh-sIt-ik |
-ic pertaining to |
Pertaining to small than normal blood cells. |
| poikilocytosis | -osis condition; usually abnormal poikil/o cyt/o |
An abnormally shaped red blood cell. |
| polycythemia vera pah-lee-sie-thEE-mee-uh vAIR-uh |
-emia blood condition poly- cyt/o |
A rare disease in which the body makes too many blood cells. |
Changes in the levels of RBCs can have significant effects on the body’s ability to effectively deliver oxygen to the tissues (Betts, et al., 2013).
Anemia
The size, shape, and number of erythrocytes, and the number of hemoglobin molecules can have a major impact on a person’s health. When the number of RBCs or hemoglobin is deficient, the general condition is called anemia. There are more than 400 types of anemia.
Anemia can be broken down into three major groups: those caused by blood loss, those caused by faulty or decreased RBC production, and those caused by excessive destruction of RBCs. In addition to these causes, various disease processes also can lead to anemias. These include chronic kidney diseases often associated with a decreased production of EPO, hypothyroidism, some forms of cancer, lupus, and rheumatoid arthritis(Betts, et al., 2013).
Blood Loss Anemias:
Causes:
- Bleeding from wounds or other lesions, including ulcers, hemorrhoids, inflammation of the stomach (gastritis), and some cancers of the gastrointestinal tract
- The excessive use of aspirin or other nonsteroidal anti-inflammatory drugs such as ibuprofen can trigger ulceration and gastritis
- Excessive menstruation and loss of blood during childbirth.
Anemias Caused by Faulty or Decreased RBC Production:
- Sickle cell anemia
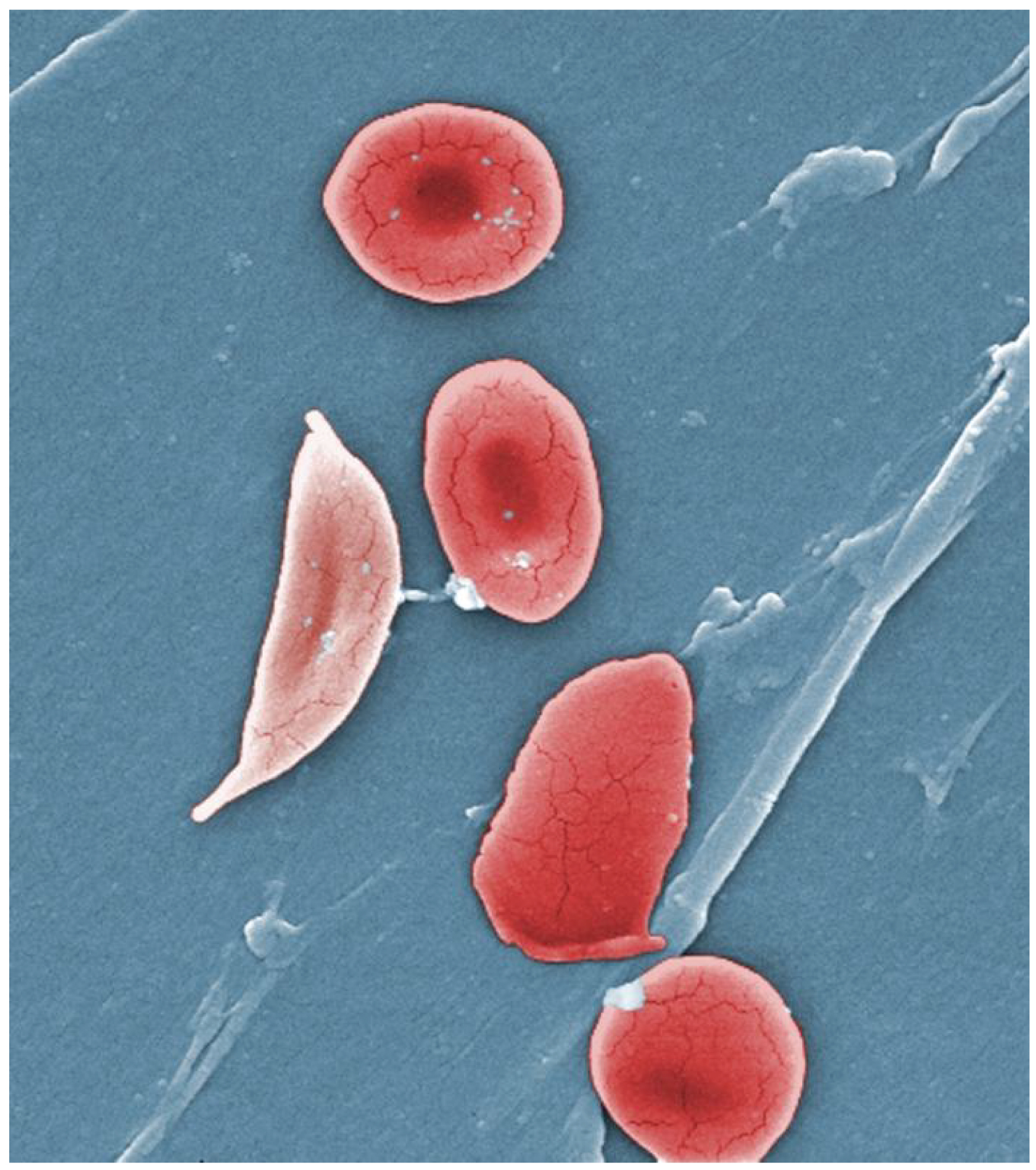
-
- A genetic disorder involving the production of an abnormal type of hemoglobin which delivers less oxygen to tissues and causes erythrocytes to assume a sickle (or crescent) shape.
- Iron deficiency anemia
- The most common type of anemia and results when the amount of available iron is insufficient to allow production of sufficient heme.
- Vitamin deficiency anemia (Generally insufficient vitamin B12 and folate).
- Megaloblastic anemia involves a deficiency of vitamin B12 and/or folate, often due to inadequate dietary intake.
- Pernicious anemia is caused by poor absorption of vitamin B12 and is often seen in patients with Crohn disease, surgical removal of the intestines or stomach (common in some weight loss surgeries), intestinal parasites, and AIDS[/pb_glossary.
- Aplastic anemia is the condition in which myeloid stem cells are defective or replaced by cancer cells, resulting in insufficient quantities of RBCs being produced. This condition by be inherited, or it may be triggered by radiation, medication, chemotherapy, or infection.
- Thalassemia is an inherited condition typically occurring in individuals from the Middle East, the Mediterranean, African, and Southeast Asia, in which maturation of the RBCs does not proceed normally. The most severe form is called Cooley’s anemia (Betts, et al., 2013).
Polycythemia
Polycythemia is an elevated RBC count and is detected in a patient’s elevated [pb_glossary id="525"]hematocrit. It can occur transiently in a person who is dehydrated; when water intake is inadequate or water losses are excessive, the plasma volume falls. As a result, the hematocrit rises. A mild form of polycythemia is chronic but normal in people living at high altitudes. Some elite athletes train at high elevations specifically to induce this phenomenon. Finally, a type of bone marrow disease called polycythemia vera causes an excessive production of immature erythrocytes. Polycythemia vera can dangerously elevate the viscosity of blood, raising blood pressure and making it more difficult for the heart to pump blood throughout the body. It is a relatively rare disease that occurs more often in men than women, and is more likely to be present in elderly patients those over 60 years of age (Betts, et al., 2013).
Leukocytes- Diseases Disorders or Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| leukemia loo-kEE-mee-uh |
-emia blood condition leuk/o |
A cancer that results in an overproduction of abnormal white blood cells. |
| mononucleosis mah-nuh-noo-klee-OH-suhs |
-osis condition mon/o one nucl/eo |
A a viral infection characterized by an abnormal increase of mononuclear white blood cells in the blood. Symptoms can include fatigue, sore throat, and swollen lymph nodes. |
| leukocytosis loo-kuh-sie-tOH-suhs |
-osis condition leuk/o cyt/o |
an increase in the number of white blood cells in the circulating blood |
| myeloma mie-uh-lOH-muh |
-oma tumor; mass; fluid collection myel/o |
A cancer that forms in a type of white blood cell called a plasma cell. Can cause can cause bone pain, weakness, and frequent infections |
Leukopenia
Leukopenia is a condition in which too few leukocytes are produced. If this condition is pronounced, the individual may be unable to ward off disease (Betts, et al., 2013).
Leukocytosis
Leukocytosis is excessive leukocyte proliferation. Although leukocyte counts are high, the cells themselves are often nonfunctional, leaving the individual at increased risk for disease (Betts, et al., 2013).
Leukemia
Leukemia is a cancer involving an abundance of leukocytes. It may involve only one specific type of leukocyte from either the myeloid line (myelocytic leukemia) or the lymphoid line (lymphocytic leukemia). In chronic leukemia, mature leukocytes accumulate and fail to die. In acute leukemia, there is an overproduction of young, immature leukocytes. In both conditions the cells do not function properly (Betts, et al., 2013).
Lymphoma
Lymphoma is a form of cancer in which masses of malignant T and/or B lymphocytes collect in lymph nodes, the spleen, the liver, and other tissues. As in leukemia, the malignant leukocytes do not function properly, and the patient is vulnerable to infection. Some forms of lymphoma tend to progress slowly and respond well to treatment. Others tend to progress quickly and require aggressive treatment, without which they are rapidly fatal (Betts, et al., 2013).
Platelet Disorders - Clotting Diseases Disorders or Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| coagulopathy | -pathy disease coagul/o |
A disease or condition affecting the blood's ability to coagulate (clot) |
| embolism Em-buh-liz-uhm |
-ism condition
embol/o |
A blocked artery caused by a foreign body, such as a blood clot or an air bubble. |
| hemophiliac hee-muh-fIl-ee-uh |
philia
hem/o |
A genetic disorder that is characterized by delayed clotting of the blood. |
| thrombocytopenia thrahm-buh-sie-tuh-pEE-nee-uh |
-penia deficiency; lack of thromb/o cyt/o |
Decrease in the number of platelets in the blood |
| thrombophilia | -philia
thromb/o |
An abnormal increase in the tendency of blood to clot and higher than normal risk of thrombosis |
| thrombosis thrahm-bOH-suhs |
-osis condition of thromb/o |
The formation or presence of a blood clot within a blood vessel |
Thrombocytosis
Thrombocytosis is a condition in which there are too many platelets. This may trigger thrombosis, a potentially fatal disorder. A thrombus (plural = thrombi) is an aggregation of platelets, erythrocytes, and even WBCs typically trapped within a mass of fibrin strands. While the formation of a clot is a normal step in hemostasis, thrombi can form within an intact or only slightly damaged blood vessel, adhering to the vessel wall and decreasing or obstructing the flow of blood. (Betts, et al., 2013).
Thrombophilia
Thrombophilia, also called hypercoagulation, is a condition in which there is a tendency to form thrombosis. This may be an inherited disorder or may be caused by other conditions including lupus, immune reactions to heparin, polycythemia vera, thrombocytosis, sickle cell disease, pregnancy, and even obesity.
When a portion of a thrombus breaks free from the vessel wall and enters the circulation, it is referred to as an embolus. An embolus that is carried through the bloodstream can be large enough to block a vessel critical to a major organ. When it becomes trapped, an embolus is called an embolism. In the heart, brain, or lungs, an embolism may accordingly cause a heart attack, a stroke, or a pulmonary embolism (Betts, et al., 2013).
Thrombocytopenia
Thrombocytopenia is a condition in which there is an insufficient number of platelets, possibly leading to ineffective blood clotting and excessive bleeding (Betts, et al., 2013).
Hemophilia
Hemophilia is a group of related genetic disorders in which certain plasma clotting factors are lacking or inadequate or nonfunctional. Patients with hemophilia bleed from even minor internal and external wounds, and leak blood into joint spaces after exercise and into urine and stool. Regular infusions of clotting factors isolated from healthy donors can help prevent bleeding in hemophiliac patients. At some point, genetic therapy will become a viable option (Betts, et al., 2013).
Plasma - Diseases, Disorders, or Conditions
| Term | Word Breakdown | Description |
|---|---|---|
| hypercalcemia hie-puhr-kal-sEE-mee-uh |
-emia blood condition hyper - |
An excess of calcium in the blood. Can lead to digestive systems, increased thirst, muscle weakness, cognitive issues, and bone pain. |
| hyperkalemia hie-puhr-kal EE-mee-uh |
-emia blood condition hyper - |
An abnormally high concentration of potassium in the blood. It can lead to heart palpitations, shortness of breath, chest pain, nausea, or vomiting. |
| hypernatremia hie-puhr-nay-tree-mee-uh |
-emia blood condition hyper - |
The presence of an abnormally high concentration of sodium in the blood. Can cause dehydration. Can cause confusion, muscle twitches, and seizures. |
| hypocalcemia hie-poh-kal-sEE-mee-uh |
-emia blood condition hypo- |
A deficiency of calcium in the blood. A deficiency of calcium in the blood. Prolonged low calcium levels can result in poor bone formation, which may result in brittle bones that are prone to fractures. |
| hypokalemia hie-poh-kay-lEE-mee-uh |
-emia blood condition hypo- |
A deficiency of potassium in the blood. A deficiency of potassium in the blood. Can cause; constipation, the feeling of skipped heart beats or palpitations, fatigue, muscle damage. Muscle weakness or spasms, Tingling or numbness Read More |
| hyponatremia hie-poh-nay-trEE-mee-uh |
-emia blood condition hypo- |
The condition of having an abnormally low level of sodium in the blood. Typically marked by nausea, vomiting, headache, confusion, fatigue, and muscle cramps and that when severe may be life-threatening if untreated |
Lymphatic and Immune Systems -Diseases Disorders or Conditions
The immune response can be under-reactive or over-reactive, leading to a state of disease. The factors that maintain immunological homeostasis are complex and incompletely understood.
| Term | Word Breakdown | Description |
|---|---|---|
| acquired immune deficiency syndrome (AIDS) uh-kwIE-uhrd i-myOOn di-fIsh-uhn-see sIn-drohm uh-kwIE-uhrd i-myOOn di-fIsh-uhn-see sIn-drohm |
HIV (human immunodeficiency virus) is a virus that attacks the body’s immune system. If HIV is not treated, it can lead to AIDS (acquired immunodeficiency syndrome). Read more and watch a video about HIV | |
| lymphadenopathy lim-fad-uh-nAH-puh-thee |
-pathy disease -lymph/o -aden/o |
Abnormal enlargement of the lymph nodes |
| lim-fi-dEE-muh lymphedema |
-edema swelling -lymph/o |
Edema due to faulty lymphatic drainage (swollen lymph nodes) |
| lymphoma lim-fOH-muh |
-oma tumor -lymph/o |
A usually malignant, cancerous tumor of lymphoid tissue |
| splenomegaly splen-oh-mEg-uh-le |
-megaly enlaregement splen/o Note there is only one "e" in the first part of the word. |
Abnormal enlargement of the spleen |
Acquired Immunodeficiency/HIV and AIDS
After seroconversion, the amount of virus circulating in the blood drops and stays at a low level for several years. During this time, the levels of CD4 T cells decline steadily, until at some point, the immune response is so weak that opportunistic disease and eventually death result.
Treatment for the disease consists of drugs that target virally encoded proteins that are necessary for viral replication but are absent from normal human cells. By targeting the virus itself and sparing the cells, this approach has been successful in significantly prolonging the lives of HIV-positive individuals (Betts, et al., 2013).
Overactive Immune System: Hypersensitivities and Autoimmune Diseases
Autoimmune Responses
The worst cases of the immune system over-reacting are autoimmune diseases in which the immune systems begin to attack cells of the patient's own body, causing chronic inflammation and significant damage. The trigger for these diseases is often unknown, although environmental and genetic factors are likely involved. Treatments are usually based on resolving the symptoms using immunosuppressive and anti-inflammatory drugs. Figure 14.15 below provides two examples of autoimmune diseases: rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) (Betts, et al., 2013).
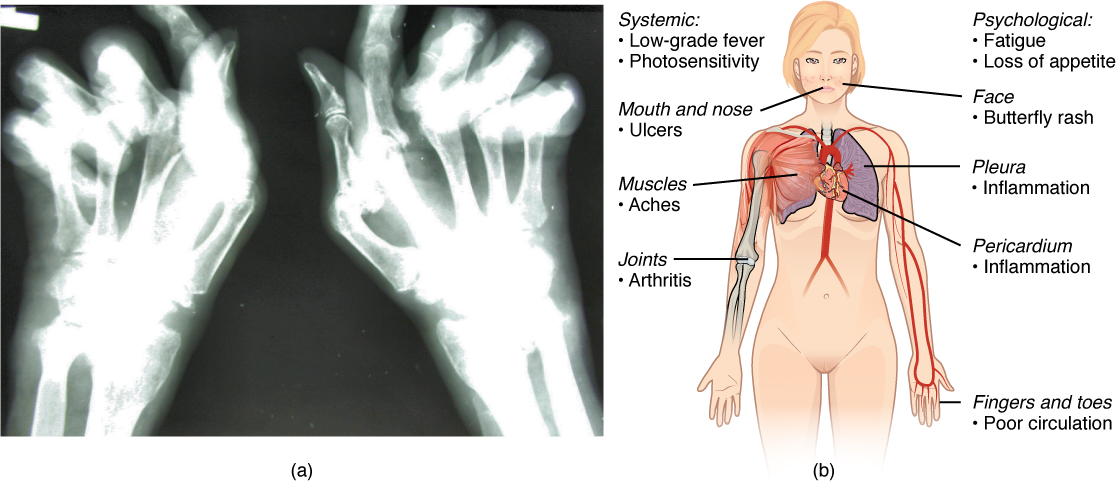
Overall, there are more than 80 different autoimmune diseases, which are a significant health problem in the elderly. Table 14.5 below lists several of the most common autoimmune diseases, the antigens that are targeted (autoantigen or "self" antigen), and the resulting tissue damage (Betts, et al., 2013).
| DISEASE | AUTOANTIGEN | SYMPTOMS |
|---|---|---|
| Celiac disease | Tissue transglutaminase | Damage to small intestine |
| Diabetes mellitus type I | Beta cells of pancreas | Low insulin production; inability to regulate serum glucose |
| Graves’ disease | Thyroid-stimulating hormone receptor (antibody blocks receptor) | Hyperthyroidism |
| Hashimoto’s thyroiditis | Thyroid-stimulating hormone receptor (antibody mimics hormone and stimulates receptor) | Hypothyroidism |
| Lupus erythematosus | Nuclear DNA and proteins | Damage of many body systems |
| Myasthenia gravis | Acetylcholine receptor in neuromuscular junctions | Debilitating muscle weakness |
| Rheumatoid arthritis | Joint capsule antigens | Chronic inflammation of joints |
Blood Lymphatic and Immune System: Medical, Surgical and Diagnostic Procedures
-
Term Word Breakdown Description bone marrow aspiration
bOHn mAIR-oh as-puhr-rAY-shuhnAspiration is a drawing of something in, out, up, or through by or as if by suction: such as the withdrawal (as by suction) of fluid or tissue from the body. A bone marrow aspiration is to collect a sample of bone marrow for analysis complete blood count (CBC)
kuhm-plEEt blUHd kOUntA complete blood count test measures the following: Red blood cells, which carry oxygen
White blood cells, which fight infection
Hemoglobin, the oxygen-carrying protein in red blood cellshematocrit
hi-mAt-uh-kruhtthe ratio (percentage) of the volume of red blood cells to the total volume of blood as determined by separation of red blood cells from the plasma usually by centrifugation immunization
im-yuh-nuh-zAY-shuhnA process by which a person becomes protected against a disease through vaccination. An immunization stimulates the body's immune response against specific diseases. morphology
mor-fAH-luh-jee-logy
study ofmorph/o
The study of the size, shape, lymphangiogram
lim-fAn-jee-uh-gram- gram
recordlymph/o
lymphangio/o
blood vesselAn x-ray of the lymph nodes and lymph vessels. The lymph nodes and vessels are not seen on a normal x-ray, so a dye or radioisotope (radioactive compound) is injected into the body to highlight the area being studied.
Read Morelymph node biopsy
lImf nOHd bIE-ahp-seeThe removal of lymph node tissue for examination under a microscope.
Read Morephlebotomy
fli-bAH-tuh-mee-otomy
incisionphleb/o
veinWhen a needle is used to take blood from a vein for medical purposes. Also called a blood draw or venipuncture. plasmapheresis
plaz-muh-fuhr-rEE-suhsThe process of obtaining plasma from blood. The process involves the following steps:
Whole blood is withdrawn from a large vein
A machine separates the liquid portion of blood (plasma) from the red and white blood cells.
The cells are transfused back along with a plasma replacement fluid.splenectomy
spli-nEk-tuh-mee-ectomy
surgical removalsplen/o
spleenA surgical removal of the spleen transfusion
trans-fyOO-zhuhnThe process of transferring blood or blood products from one person to another autologous transfusion
aw-tAH-luh-guhsaut/o
selfA transfusion where the individual as both donor and recipient vaccination
vak-suh-nAY-shuhnIntroducing harmless fragments of pathogens to activate the immune response —the presence of a disease-causing organism in the body—to engage the body’s natural defenses. The active ingredient in all vaccines is an antigen, the name for any substance that causes the immune system to begin producing antibodies. In a vaccine, the antigen could help guard against
1) Viruses, like the ones that cause the flu and COVID-19
2) Bacterial infection , including tetanus, diphtheria, and pertussisVaccines can help prevent
1) Viruses, like the ones that cause the flu and COVID-19
2) Bacterial infection , including tetanus, diphtheria, and pertussisvenipuncture
vEE-nuh-puhng-chuhrSurgical puncture of a vein especially for the withdrawal of blood or for intravenous medication Blood Lymphatic and Immune System: Drug Categories
Term Word Breakdown Description anticoagulant
an-tie-koh-Ag-yuh-luhnt-ant
pertaining toanti- against
coagul/o
clottingMedication that prevents blood clots erythropoietin
i-rith-roh-pOI-uh-tuhn-poietin
subtance that fromserythr/o
redA substance that forms red blood cells – stimulates the red marrow to make erythrocytes immunosuppressant
im-yuh-noh-suh-prEs-ntImmunosuppressant is a class of medicines that inhibit or decrease the intensity of the immune response in the body. thrombolytic enzyme
thrahm-buh-lIt-ik En-ziemz-ic
pertaining tothromb/o
blood clotDrugs that dissolve a major clot quickly.
Medical Specialties Related to Blood, the Lymphatic or Immune Systems
| Term | Word Breakdown | Description |
|---|---|---|
| hematologist HEE-muh-TAH-loh-jist |
-logist one who studies hemat/o |
A doctor who has special training in diagnosing and treating blood disorders. |
| phlebotomist fli-bAH-tuh-mist |
-ist specialist phleb/o tom/o |
Phlebotomists primarily draw blood, which is then used for different kinds of medical laboratory testing or for procedures, such as transfusions. In medical and diagnostic laboratories, patients sometimes interact only with the phlebotomist. |
| Medical Lab Technologist | Technologist that performs complex analyses of tissue, blood and other body fluids. |
Medical Laboratory Technologist
Medical or clinical laboratories employ a variety of individuals in technical positions.
- Medical laboratory technologists (MLT) perform complex analyses of tissue, blood and other body fluids.
Review the requirements of the MLT degree at Tulsa Community College
Immunology is a medical specialty that diagnoses and treats diseases of the immune system
Skin testing (for allergies) is done by a clinical immunologist/allergist to identify allergens in Type I hypersensitivity. In skin testing, allergen extracts are injected into the epidermis, and a positive result of the wheal and flare response usually occurs within 30 minutes. The soft center is due to fluid leaking from the blood vessels and the redness is caused by the increased blood flow to the area that results from the dilation of local blood vessels at the site (Betts, et al., 2013).
-
-
-
-
Test Yourself
References
Canadian Medical Association. (2018, August). Clinical immunology/allergy profile. Canadian Medical Association Specialty Profiles. https://www.cma.ca/sites/default/files/2019-01/immunology-allergy-e.pdf.
Canadian Medical Association. (2018, August). Hematology profile. CMA Specialty Profiles. https://www.cma.ca/sites/default/files/2019-01/hematology-e.pdfCanadian Society for Medical Laboratory Science. (n.d.). Who are lab professionals. https://www.csmls.org/Medical-Laboratory-Professionals/About/Who-are-Lab-Professionals.aspxSonography Canada. (2020). Credentials. https://sonographycanada.ca/certification/credentials Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
-
-
-
Image Descriptions
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
A centrifuge is a common piece of laboratory equipment used to spin test tubes at a high speed in order to separate components in a liquid by weight.
red blood cells
also spelled leucocyte, these are white blood cells
also called platelets, these are cell fragments that aid in blood clotting
A lab test which measures the percentage red blood cells in a sample of whole blood. It represents how much of the person's blood is made up of red blood cells, by volume.
Blood clotting cells also called thrombocytes.
also called hematopoiesis; from the Greek root haima- = “blood”; -poiesis = “production”
also phagocytosed, this is the process by which certain cells are able to 'eat' other cells or substances by engulfing them
a type of leukocyte (usually a monocyte) that has the ability to ingest and destroy other cells or pathogens
excessive or uncontrolled bleeding from the blood vessels
pH is a measure of how acidic or alkaline a substance is, as determined by the number of free hydrogen ions in the substance.
the process by which the body seals a ruptured blood vessel to prevent further blood loss
hypo=below, lower than normal, volemic=pertaining to volume (in this case, the volume of blood in the body)
Cardio=pertaining to the heart
genic=originating from, created by
Cardiogenic means originating from the heart
A piece of a blood clot or other substance has broken free from its original location and traveled through the bloodstream to lodge in a smaller vessel in the lungs. This causes an obstruction in that vessel and hypoxia to the tissues supplied by that vessel.
The pericardial sac surrounding the heart has filled with blood or other fluid and the resulting pressure is preventing the heart from beating effectively
An excessive amount of air is present in the thoracic cavity, outside of the lungs, putting pressure on the lungs and interfering with venous return, pulmonary function, and delivery of oxygen to the tissues
Erythropoietin is a hormone produced by the kidneys that plays an important role in the homeostasis of red blood cells levels in the body
Underactive thyroid gland, insufficient production of thyroid hormones (T3 and T4)
An autoimmune disease in which the body mounts an immune response against its own tissues, causing chronic inflammation and tissue damage
An autoimmune disorder in which the body mounts an immune response against its own joint tissues, causing inflammation and damage to the joints
A type of inflammatory bowel disease
Acquired immunodeficiency syndrome, caused by infection with the HIV virus
Viscosity is the thickness of fluids that affects their ability to flow
formation of unwanted blood clots
A type of bone marrow disease that causes an excessive production of immature erythrocytes
A condition in which there are too many platelets
Also called sickle cell anemia: A genetic disorder involving the production of an abnormal type of hemoglobin which delivers less oxygen to tissues and causes erythrocytes to assume a sickle (or crescent) shape
Human Immunodeficiency Virus. An infectious disease, usually transmitted via blood or sexual fluids. It attacks the immune system and can lead to full-blown AIDS
Seroconversion is the reciprocal relationship between virus levels in the blood and antibody levels. As the antibody levels rise, the virus levels decline, and this is a sign that the immune response is being at least partially effective. Partially, because in many diseases, seroconversion does not necessarily mean a patient is getting well.(Betts et al., 2013)
CD4 is the receptor that HIV uses to get inside T cells and reproduce. CD4+ helper T cells play an important role in T cell immune responses and antibody responses. (Betts et al., 2013)
a soft, pale swelling at the site surrounded by a red zone (Betts et al., 2013)