12 Endocrine System
Learning Objectives
- Identify the anatomy of the endocrine system
- Describe the main functions of the endocrine system
- Spell the medical terms of the endocrine system and use correct abbreviations
- Identify the medical specialties associated with the endocrine system
- Explore common diseases, disorders, and procedures related to the endocrine system
Chapter Twelve: Table of Contents
What is it?
What Can Go Wrong? – Diseases, Disorders, and Conditions of the Endocrine System
How Do We Fix it or Make it Better?
- Laboratory and Diagnostic Tests
- Surgical Procedures
- Drug Categories
Test Yourself
References, Attributions, and Image Descriptions
General Terms
| Term | Word Breakdown | Description |
|---|---|---|
| endocrinology en-duh-kri-nAH-luh-jee En-duh-kruhn glAnd |
-logy study of endo- crin/o |
The branch of medicine that studies the production and regulation of hormones |
| endocrine gland
|
endo- within; inner crin/o |
Glands that secrete hormones directly into the bloodstream, |
| exocrine gland Ek-suh-kruhn glAnd |
exo- outer; outside crin/o crin/o |
Glands that secrete substances through ducts to specific target areas. |
Endocrine System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Endocrine System.
Return to the Table of Contents
Introduction to Endocrine System
- Glands located throughout the body;
- Hormones made by the glands and released into the bloodstream or the fluid surrounding cells; and
- Receptors in various organs and tissues that recognize and respond to the hormones.
Why are Hormones Important?
Hormones act as chemical messengers that are released into the blood stream to act on an organ in another part of the body. Although hormones reach all parts of the body, only target cells with compatible receptors are equipped to respond. Over 50 hormones have been identified in humans and other vertebrates.
Hormones control or regulate many biological processes and are often produced in exceptionally low amounts within the body. Examples of such processes include:
- blood sugar control (insulin);
- differentiation, growth, and function of reproductive organs (testosterone and estradiol); and
- body growth and energy production (growth hormone and thyroid hormone).
Much like a lock and key, many hormones act by binding to receptors that are produced within cells. When a hormone binds to a receptor, the receptor carries out the hormone's instructions, either by altering the cell's existing proteins or turning on genes that will build a new protein. The hormone-receptor complex switches on or switches off specific biological processes in cells, tissues, and organs.
Some examples of hormones include:
- Estrogens are the group of hormones responsible for female sexual development. They are produced primarily by the ovaries and in small amounts by the adrenal glands.
- Androgens are responsible for male sex characteristics. Testosterone, the sex hormone produced by the testicles, is an androgen.
- The thyroid gland secretes two main hormones, thyroxine and triiodothyronine, into the bloodstream. These thyroid hormones stimulate all the cells in the body and control biological processes such as growth, reproduction, development, and metabolism.
The endocrine system, made up of all the body's different hormones, regulates all biological processes in the body from conception through adulthood and into old age, including the development of the brain and nervous system, the growth and function of the reproductive system, as well as the metabolism and blood sugar levels. The female ovaries, male testes, and pituitary, thyroid, and adrenal glands are major constituents of the endocrine system.
Watch this video:
Media 20.1 Endocrine System, Part 1 - Glands & Hormones: Crash Course A&P #23 [Online video]. Copyright 2015 by CrashCourse.
Endocrine System Medical Terms
Return to the Table of Contents
Anatomy (Structures) of the Endocrine System
The ductless endocrine glands are not to be confused with the body’s exocrine system, whose glands release their secretions through ducts. Examples of exocrine glands include the sebaceous and sweat glands of the skin
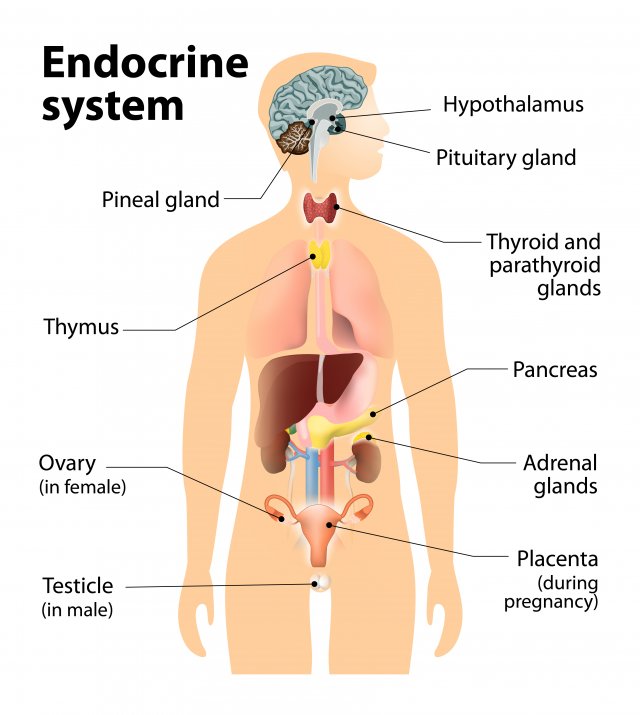
Hypothalamus - The hypothalamus links our endocrine and nervous systems together. The hypothalamus drives the endocrine system.
Pituitary gland - The pituitary gland receives signals from the hypothalamus. This gland has two lobes, the posterior and anterior lobes. The posterior lobe secretes hormones that are made by the hypothalamus. The anterior lobe produces its own hormones, several of which act on other endocrine glands.
Thyroid gland - The thyroid gland is critical to the healthy development and maturation of vertebrates and regulates metabolism.
Adrenal glands - The adrenal gland is made up of two glands: the cortex and medulla. These glands produce hormones in response to stress and regulate blood pressure, glucose metabolism, and the body's salt and water balance.
Pancreas - The pancreas is responsible for producing glucagon and insulin. Both hormones help regulate the concentration of glucose (sugar) in the blood.
Gonads - The male reproductive gonads, or testes, and female reproductive gonads, or ovaries, produce steroids that affect growth and development and also regulate reproductive cycles and behaviors. The major categories of gonadal steroids are androgens, estrogens, and progestins, all of which are found in both males and females but at different levels.
| Endocrine Gland | Associated Hormones | Chemical Class | Effect |
|---|---|---|---|
| Pituitary (anterior) | Growth hormone (GH) | Protein | Promotes growth of body tissues |
| Pituitary (anterior) | Prolactin (PRL) | Peptide | Promotes milk production |
| Pituitary (anterior) | Thyroid-stimulating hormone (TSH) | Glycoprotein | Stimulates thyroid hormone release |
| Pituitary (anterior) | Adrenocorticotropic hormone (ACTH) | Peptide | Stimulates hormone release by adrenal cortex |
| Pituitary (anterior) | Follicle-stimulating hormone (FSH) | Glycoprotein | Stimulates gamete production |
| Pituitary (anterior) | Luteinizing hormone (LH) | Glycoprotein | Stimulates androgen production by gonads |
| Pituitary (posterior) | Antidiuretic hormone (ADH) | Peptide | Stimulates water reabsorption by kidneys |
| Pituitary (posterior) | Oxytocin | Peptide | Stimulates uterine contractions during childbirth |
| Thyroid | Thyroxine (T4), triiodothyronine (T3) | Amine | Stimulate basal metabolic rate |
| Thyroid | Calcitonin | Peptide | Reduces blood Ca2+ levels |
| Parathyroid | Parathyroid hormone (PTH) | Peptide | Increases blood Ca2+ levels |
| Adrenal (cortex) | Aldosterone | Steroid | Increases blood Na+ levels |
| Adrenal (cortex) | Cortisol, corticosterone, cortisone | Steroid | Increase blood glucose levels |
| Adrenal (medulla) | Epinephrine, norepinephrine | Amine | Stimulate fight-or-flight response |
| Pineal | Melatonin | Amine | Regulates sleep cycles |
| Pancreas | Insulin | Protein | Reduces blood glucose levels |
| Pancreas | Glucagon | Protein | Increases blood glucose levels |
| Testes | Testosterone | Steroid | Stimulates development of male secondary sex characteristics and sperm production |
| Ovaries | Estrogens and progesterone | Steroid | Stimulate development of female secondary sex characteristics and prepare the body for childbirth |
Regulation of Hormone Secretion
To prevent abnormal hormone levels and a potential disease state, hormone levels must be tightly controlled. The body maintains this control by balancing hormone production and degradation. Feedback loops govern the initiation and maintenance of most hormone secretion in response to various stimuli.
Effects of Endocrine Disruption
In the last two decades there has been a growing awareness of the possible adverse effects in humans a nd wildlife from exposure to chemicals t hat can interfere with the endocrine system. These effects can include:
- developmental malformations;
- interference with reproduction;
- increased cancer risk; and
- disturbances in the immune and nervous system function.
Clear evidence exists that some chemicals cause these effects in wildlife, but limited evidence exists for the potential of chemicals to cause these effects in humans at environmental exposure levels. Very few chemicals have been tested for their potential to interfere with the endocrine system. Current standard test methods do not provide adequate data to identify potential endocrine disruptors (EDs) or to assess their risks to humans and wildlife.
How Chemicals Can Disrupt the Endocrine System
Scientific research on human epidemiology, laboratory animals, and fish and wildlife suggests that environmental contaminants can disrupt the endocrine system, leading to adverse health consequences.
It is important to gain a better understanding of what concentrations of chemicals found in the environment may cause an adverse effect. Various types of scientific studies (e.g., epidemiology, mammalian toxicology, and ecological toxicology) are necessary to resolve uncertainty surrounding endocrine disruption. Many such studies are underway by government agencies, industry and academia.
Disruption of the endocrine system can occur in various ways. Some chemicals mimic a natural hormone, fooling the body into over-responding to the stimulus (e.g., a growth hormone that results in increased muscle mass), or responding at inappropriate times (e.g., producing insulin when it is not needed). Other endocrine disruptors block the effects of a hormone from certain receptors (e.g., growth hormones required for normal development). Still others directly stimulate or inhibit the endocrine system and cause overproduction or underproduction of hormones (e.g. an over or underactive thyroid).
Certain drugs are used to intentionally cause some of these effects, such as birth control pills. In many situations involving environmental chemicals, however, an endocrine effect is not desirable.
Examples of Endocrine Disruption
One example of the devastating consequences of the exposure of developing animals, including humans, to endocrine disruptors is the case of the potent drug diethylstilbestrol (DES), a synthetic estrogen. Prior to its ban in the early 1970s, doctors mistakenly prescribed DES to as many as five million pregnant women to block spontaneous abortion and promote fetal growth. It was discovered after the children went through puberty that DES affected the development of the reproductive system and caused vaginal cancer.
Since then, Congress has improved the evaluation and regulation of drugs and other chemicals. The statutory requirement to establish an endocrine disruptor screening program is a highly significant step.
Growing scientific evidence shows that humans, domestic animals, and fish and wildlife species have exhibited adverse health consequences from exposure to environmental chemicals that interact with the endocrine system. To date, such problems have been detected in domestic or wildlife species with relatively high exposure to:
- organochlorine compounds (e.g., 1,1,1- trichloro-2,2-bis(p-chlorophenyl);
- ethane (DDT) and its metabolite dichorodiphenyldichloroethylene (DDE);
- polychlorinated biphenyls (PCBs), and dioxins); and
- some naturally occurring plant estrogens.
Effects from exposure to low levels of endocrine disruptors have been observed as well (e.g., parts-per-trillion levels of tributyl tin have caused masculinization of female marine molluscs such as the dog whelk and ivory shell). Adverse effects have been reported for humans exposed to relatively high concentrations of certain contaminants. However, whether such effects are occurring in the human population at large at concentrations present in the ambient environment, drinking water, and food remains unclear.
Several conflicting reports have been published concerning declines in the quality and quantity of sperm production in humans over the last four decades, and there are reported increases in certain cancers (e.g., breast, prostate, testicular). Such effects may have an endocrine-related basis, which has led to speculation about the possibility that these endocrine effects may have environmental causes. However, considerable scientific uncertainty remains regarding the actual causes of such effects.
Nevertheless, there is little doubt that small disturbances in endocrine function, particularly during certain highly sensitive stages of the lifecycle (e.g., development, pregnancy, lactation) can lead to profound and lasting effects.
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Endocrine System
Diseases, Disorders, and Conditions of the Pituitary Gland
| Term | Word Breakdown | Description |
|---|---|---|
| acromegaly ak-roh-mEg-uh-lee |
-megaly enlargement acr/o |
Enlargement of certain body parts, such as the hands, feet, and facial bones after the closure of the growth plates. Differs from gigantism that occurs during childhood or adolescence, when the growth plates are open. |
| adenoma ad-uh-nOH-muh |
-oma tumor; mass; fluid collection aden/o |
Benign tumor in the pituitary gland. Pituitary adenomas can cause various hormonal imbalances and lead to conditions such as hyperpituitarism, hypopituitarism, gigantism, acromegaly, and other pituitary gland disorders. |
| dwarfism dwOR-fiz-uhm |
-ism condition dwarf |
Abnormally short stature that can be caused by partial or complete growth hormone deficiency |
| galactorrhea guh-lak-tuhr-rEE-uh |
-rrhea flow or discharge galact/o |
A condition where there is an excessive production and discharge of milk from the breast in individuals who are not breastfeeding. |
| gigantism jie-gAn-tiz-uhm |
-ism condition gigant/o |
A rare condition typically caused by the overproduction of growth hormone (GH) during childhood or adolescence. It leads to excessive growth and an abnormal increase in height. Differs from acromegaly that causes excessive growth in the extremities after the growth plates are closed. |
| hyperpituitarism hie-puhr-puh-tOO-uh-tuhr-riz-uhm |
-ism condition hyper- pituitar/o |
A condition characterized by excessive secretion of one or more pituitary hormones. It is usually caused by a pituitary adenoma, a benign tumor in the pituitary gland. The overproduction of hormones can lead to various symptoms and complications such as gigantism, acromegaly, and hormonal imbalances. |
| hypopituitarism hie-poh-puh-tOO-uh-tuhr-riz-uhm |
-ism condition hypo- pituitar/o |
A condition characterized by deficient hormone production by the pituitary gland. This can lead to a range of symptoms, including growth hormone deficiency, thyroid hormone deficiency, adrenal insufficiency, and reproductive hormone imbalances. The consequences of hypopituitarism can include stunted growth, fatigue, weight gain, infertility, and disruption of various bodily functions. |
| panhypopituitarism pan-hie-poh-puh-tOO-uh-tuhr-riz-uhm |
-ism condition pan- hypo- pituitar/o |
A condition where all pituitary hormone production is reduced or absent. It can be caused by pituitary tumors, radiation therapy, severe head trauma, or certain genetic conditions. Symptoms of panhypopituitarism may include fatigue, weight loss, low blood pressure, delayed puberty, and loss of appetite. |
| diabetes insipidus die-uh-bEE-teez |
A disorder of the pituitary gland characterized by intense thirst and by the excretion of large amounts of urine | |
| polydipsia pah-lee-dIp-see-uh |
-ia condition poly- dips/o |
Excessive thirst |
| polyuria pah-lee-yUR-ee-uh |
-ia condition poly- ur/o |
Excessive secretion of urine |
Return to the Table of Contents
-
Diseases, Disorders, and Conditions of the Thyroid Gland
Term Word Breakdown Description cretinism
krEE-tn-iz-uhm-ism
conditioncretin
a dwarfed deformed idiot (https://www.etymonline.com/search?q=cretinism)A condition of severely stunted physical and mental growth due to untreated deficiency of thyroid hormone during fetal development and infancy. exophthalmos
ek-sahf-thAl-muhsopthalm/o
eyeex- outward
Bulging eyes (exophthalmos) are be a sign of a problem with the thyroid gland. It can be treated, but needs to be checked quickly vision can be affected. goiter (thyromegaly)
gOI-tuhrEnlargement of the thyroid gland, typically due to iodine deficiency or certain thyroid disorders. Grave’s disease
grAYvz di-zEEzAn autoimmune disorder characterized by the overproduction of thyroid hormones. It is the most common cause of hyperthyroidism. It leads to the growth of the thyroid gland (resulting in goiter) and increased production of thyroid hormones. Clinical features of Graves' disease include hyperthyroidism symptoms such as weight loss, rapid heartbeat, heat intolerance, and exophthalmos (bulging eyes). hyperthyroidism
hie-puhr-thIE-roi-diz-uhm-ism
conditionhyper-
above; beyond; excessivethyr/o
thyroid glandExcessive production of thyroid hormones leading to increased metabolic rate and symptoms like weight loss, rapid heartbeat, and heat intolerance. hypothyroidism (Hashimoto’s thyroiditis)
hie-poh-thIE-roi-diz-uhm-ism
conditionhypo-
under; deficientthyr/o
thyroid glandA condition characterized by an underactive thyroid gland, resulting in insufficient production of thyroid hormones. Clinical manifestations of hypothyroidism include fatigue, weight gain, cold intolerance, dry skin, and depression. myxedema
mik-suh-dEE-muhA severe form of hypothyroidism characterized by dry and pale skin, puffy face, and slowed mental function thyroid carcinoma
thIE-roid kahr-suh-nOH-muh-oid
resemblingthyr/o
thyroid gland-oma
tumor; mass; fluid collectioncarcin/o
cancerA cancerous tumor originating from the cells of the thyroid gland. thyrotoxicosis
thie-roh-tahk-suh-kOH-suhs-osis
conditionthyr/o
thyroid glandtoxic/o
poisonExcessive circulating thyroid hormones, regardless of the cause. Symptoms of overt thyrotoxicosis include heat intolerance, palpitations, anxiety, fatigue, weight loss, muscle weakness, and, in women, irregular menses.
Diseases, Disorders, and Conditions of the Parathyroid Gland
| Term | Word Breakdown | Description |
|---|---|---|
| hypercalcemia hie-puhr-kal-sEE-mee-uh |
-emia blood condition hyper- calc/o |
An excess of calcium in the blood |
| hypocalcemia hie-poh-kal-sEE-mee-uh |
-emia blood condition hypo- calc/o |
A deficiency of calcium in the blood |
| hypoparathyroidism hIE-poh-par-uh-thIE-roi-diz-uhm |
-ism condition hypo- para- thyr/o |
An endocrine disorder that is marked by a deficiency of parathyroid hormone resulting in hypocalcemia and that is characterized especially by muscle weakness and cramps, tingling or numbness of the lips, hands, or feet, and sometimes muscle spasms |
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Adrenal Gland, Cortex and Androgens
| Term | Word Breakdown | Description |
|---|---|---|
| hyperaldosteronism hie-pUHR-al-DOS-teh-rone-niz-uhm |
-ism condition hyper- |
Aldosterone is a steroid hormone made by the adrenal cortex (the outer layer of the adrenal gland). It helps control the balance of water and salts in the kidney by keeping sodium in and releasing potassium from the body. Too much aldosterone can cause high blood pressure and a build-up of fluid in body tissues. |
| Addison's Disease Ad-uh-suhnz di-zEEz |
Addison's disease is primarily caused by autoimmune destruction of the adrenal glands. The main symptoms of Addison's disease include fatigue, weight loss, muscle weakness, low blood pressure, darkening of the skin, and salt craving. | |
| Cushing’s Syndrome kUsh-ingz sIn-drohm |
Characterized by a collection of signs and symptoms that occur due to prolonged exposure to high levels of cortisol. The main symptoms include weight gain, particularly in the abdominal area, thinning skin, easy bruising, muscle weakness, fatigue, and mood swings | |
| hirsutism hUHR-suh-tiz-uhm |
-ism condition hirsut/o |
Condition where women have thick, dark hair on their face, neck, chest, tummy, lower back, buttocks or thighs. |
| virilism vIR-uh-liz-uhm |
-ism condition viril/o |
The appearance of male secondary sex characteristics (such as facial hair) in the female |
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Pineal
| Term | Word Breakdown | Description |
|---|---|---|
| Seasonal Affective Disorder (SAD) | A recurrent major depressive disorder with a seasonal pattern usually beginning in fall and continuing into winter months. People with SAD may have difficulty with overproduction of melatonin. Melatonin is a hormone produced by the pineal gland that responds to darkness by causing sleepiness. |
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Pancreas
| Term | Word Breakdown | Description |
|---|---|---|
| diabetesmellitus (DM) ie-uh-bEE-teez mEl-it-uhs |
Disease where your pancreas doesn’t make insulin or makes very little insulin. Insulin helps blood sugar enter the cells in your body for use as energy. Without insulin, blood sugar can’t get into cells and builds up in the bloodstream. High blood sugar is damaging to the body and causes many of the symptoms and complications of diabetes. | |
| glycosuria glie-koh-shUR-ee-uh |
-ia condition glyc/o |
Excess of sugar in the urine |
| hyperglycemia hie-puhr-glie-sEE-mee-uh |
-emia blood condition hyper- glyc/o |
Excess of sugar in the blood |
| hypoglycemia hie-poh-glie-sEE-mee-uh |
-emia blood condition hypo- glyc/o |
Abnormal decrease of sugar in the blood |
| ketoacidosis | -osis condition keto/o acid |
Resulting from increased levels of ketone bodies in the blood Ketoacidosis occurs most commonly as a complication of diabetes but may occur from other causes (such as starvation). Read more |
| polyphagia pah-lee-fAY-juh |
-ia condition poly- phag/o |
Excessive appetite or eating |
| nephropathy ni-frAH-puh-thee |
-pathy disease nephr/o |
Kidney disease (a complication of diabetes) |
| neuropathy nu-rAH-puh-thee |
-pathy disease neur/o |
Damage, disease, or dysfunction of one or more nerves (a complication of diabetes) |
| retinopathy ret-uh-nAH-puh-thee |
-pathy disease retin/o |
Disorders of the retina including some that cause blindness (a complication of diabetes) |
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Testes
| Term | Word Breakdown | Description |
|---|---|---|
| precocious puberty pri-kOH-shuhs pyOO-buhr-tee |
Early puberty, also called precocious puberty, is when:
girls have signs of puberty before 8 years of age Can come from hormonal imbalances that simulate the ovaries and testes. |
|
| gynecomastia gie-nuh-koh-mAs-tee-uh |
-ia condition gynec/o mast/o |
A common condition that causes boys' and men's breasts to swell and become larger than normal. (sometimes referred to as "man boobs"). It is most common in teenage boys and older men Read more |
Return to the Table of Contents
Diseases, Disorders, and Conditions of the Ovaries
| Term | Word Breakdown | Description |
|---|---|---|
| menopause mEn-uh-pawz |
-pause a halt, stop, cessation men/o |
The natural cessation (stopping) of menstruation that usually occurs between the ages of 45 and 55. Triggered by hormonal changes |
Return to the Table of Contents
Laboratory and Diagnostic Procedures
| Term | Word Breakdown | Description |
|---|---|---|
| fasting blood sugar (FBS) | A blood test used to find out if your blood sugar levels are in a healthy range. It is often used to help diagnose and monitor diabetes. | |
| glucose tolerance test (GTT) | A lab test to check how your body moves sugar from the blood into tissues like muscle and fat. The test is often used to diagnose diabetes. Read more | |
| urine dipstick | A dipstick is a thin, plastic stick with strips of chemicals on it. A nurse or technician puts it into the urine sample. Then, its chemical patches will change color if the sample contains things like white blood cells, protein, or glucose. |
Return to the Table of Contents
Surgical Procedures
| Term | Word Breakdown | Description |
|---|---|---|
| adrenalectomy uh-dree-nuh-lEk-tuh-mee |
-ectomy surgical removal adren/o |
Procedure to remove a diseased or cancerous adrenal gland. Adrenal glands help regulate your metabolism, immune system, blood pressure, response to stress and other essential functions. |
| parathyroidectomy par-uh-thie-roi-dEk-tuh-mee |
-ectomy surgical removal para-
thyr/o |
A surgery to remove the parathyroid glands or parathyroid tumors. The parathyroid glands are right behind your thyroid gland in your neck. These glands help your body control the calcium level in the blood. |
| thyroidectomy thie-roi-dEk-tuh-mee |
-ectomy surgical removal thyr/o |
A procedure used to excise (remove) the thyroid gland. It is a common procedure in modern medicine and may be used to treat malignancy, benign disease, or hormonal disease that is not responsive to medical management |
Endocrinology Careers
Endocrinologists—medical doctors who specialize in this field—are experts in treating diseases associated with hormonal systems, ranging from thyroid disease to diabetes. Endocrine surgeons treat endocrine disease through the removal of the affected endocrine gland or tissue. Some patients experience health problems as a result of the normal decline in hormones that can accompany aging. These patients can consult with an endocrinologist to weigh the risks and benefits of hormone replacement therapy intended to boost their natural levels of reproductive hormones. In addition to treating patients, endocrinologists may be involved in research to improve the understanding of endocrine system disorders and develop new treatments for these diseases (Betts, et al., 2013).
- A thyroid specialist is an endocrinologist whose sub specialty is focused on the treatment and disorders of the thyroid gland such as hypothyroidism (too low secretion) and hyperthyroidism (too high secretion).
- A diabetes specialist is an endocrinologist whose sub specialty is focused on the treatment of diabetic conditions.
References
[CrashCourse]. (2015, June 22). Endocrine system, part 1 - glands & hormones: Crash course A&P #23 [Video]. YouTube. https://www.youtube.com/watch?v=eWHH9je2zG4
[CrashCourse]. (2015, June 29). Endocrine system, part 2 - hormone cascade: Crash course A&P #24 [Video]. YouTube. https://www.youtube.com/watch?v=eWHH9je2zG4
Giorgi, A., & Cherney, K. (2018). Thyroid scan. Healthline. https://www.healthline.com/health/thyroid-scan
MedlinePlus. (2020). Radioactive iodine uptake. US National Library of Medicine. https://medlineplus.gov/ency/article/003689.htm
Shurkin, J.N.(2013, August 2). Trouble sleeping? Go camping: Artificial light sources can negatively affect circadian rhythms, scientists say. Scientific American. https://www.scientificamerican.com/article/trouble-sleeping-go-campi/
[TravelersDefense]. (2009, July 28). What does melatonin do? Melatonin use info [Video]. YouTube. https://www.youtube.com/watch?v=EUyBDGgsk_I
Image Descriptions
Figure 20.1 image description: This photo shows a young girl reaching for an orange leaf on an oak tree. She is on a walkway near a creek. The opposite shore is a deep slope covered with more trees in autumn colors. [Return to Figure 20.1].
Figure 20.2 image description: This diagram shows the endocrine glands and cells that are located throughout the body. The endocrine system organs include the pineal gland and pituitary gland in the brain. The pituitary is located on the anterior side of the thalamus while the pineal gland is located on the posterior side of the thalamus. The thyroid gland is a butterfly-shaped gland that wraps around the trachea within the neck. Four small, disc-shaped parathyroid glands are embedded into the posterior side of the thyroid. The adrenal glands are located on top of the kidneys. The pancreas is located at the center of the abdomen. In females, the two ovaries are connected to the uterus by two long, curved, tubes in the pelvic region. In males, the two testes are located in the scrotum below the penis. [Return to Figure 20.2].
Figure 20.3 image description: This diagram shows a negative feedback loop using the example of glucocorticoid regulation in the blood. Step 1 in the cycle is when an imbalance occurs. The hypothalamus perceives low blood concentrations of glucocorticoids in the blood. This is illustrated by there being only 5 glucocorticoids floating in a cross section of an artery. Step 2 in the cycle is hormone release, where the hypothalamus releases corticotropin-releasing hormone (CRH). Step 3 is labeled correction. Here, the CRH release starts a hormone cascade that triggers the adrenal gland to release glucocorticoid into the blood. This allows the blood concentration of glucocorticoid to increase, as illustrated by 8 glucocorticoid molecules now being present in the cross section of the artery. Step 4 is labeled negative feedback. Here, the hypothalamus perceives normal concentrations of glucocorticoids in the blood and stops releasing CRH. This brings blood glucocorticoid levels back to homeostasis. [Return to Figure 20.3].
Figure 20.4 image description: This illustration zooms in on the hypothalamus and the attached pituitary gland. The anterior pituitary is highlighted. Three neurosecretory cells are secreting hormones into a web-like network of arteries within the infundibulum. The artery net is labeled the primary capillary plexus of the hypophyseal portal system. The superior hypophysel artery enters the primary capillary plexus from outside of the infundibulum. The hypophyseal portal vein runs down from the primary capillary plexus, through the infundibulum, and connects to the secondary capillary plexus of the hypophyseal portal system. The secondary capillary plexus is located within the anterior pituitary. The hormones released from the neurosecretory cells of the hypothalamus travel through the primary capillary plexus, down the hypophyseal portal vein, and into the secondary capillary plexus. There, the hypothalamus hormones stimulate the anterior pituitary to release its hormones. The anterior pituitary hormones leave the primary capillary plexus from a single vein at the bottom of the anterior lobe. [Return to Figure 20.4].
Figure 20.5 image description: This flow chart illustrates the hormone cascade that stimulates human growth. In step 1, the hypothalamus releases growth hormone-releasing hormone (GHRH). GHRH travels into the primary capillary plexus of the anterior pituitary, where it stimulates the anterior pituitary to release growth hormone (GH). The release of growth hormone causes three types of effects. In the glucose-sparing effect, GH stimulates adipose cells to break down stored fat, fueling the growth effects (discussed next). The target cells for the glucose-sparing effects are adipose cells. In the growth effects, GH increases the uptake of amino acids from the blood and enhances cellular proliferation while also reducing apoptosis. The target cells for the growth effects are bone cells, muscle cells, nervous system cells, and immune system cells. In the diabetogenic effect, GH stimulates the liver to break down glycogen into glucose, fueling the growth effects. The liver also releases IGF in response to GH. The IGF further stimulates the growth effects but also negatively feeds back to the hypothalamus. When high IGF one levels are perceived by the hypothalamus, it releases growth hormone inhibiting hormone (GHIH). GHIH inhibits GH release by the anterior pituitary. [Return to Figure 20.5].
Figure 20.6 image description: This illustration zooms in on the hypothalamus and the attached pituitary gland. The posterior pituitary is highlighted. Two nuclei in the hypothalamus contain neurosecretory cells that release different hormones. The neurosecretory cells of the paraventricular nucleus release oxytocin (OT) while the neurosecretory cells of the supraoptic nucleus release anti-diuretic hormone (ADH). The neurosecretory cells stretch down the infundibulum into the posterior pituitary. The tube-like extensions of the neurosecretory cells within the infundibulum are labeled the hypothalamophypophyseal tracts. These tracts connect with a web-like network of blood vessels in the posterior pituitary called the capillary plexus. From the capillary plexus, the posterior pituitary secretes the OT or ADH into a single vein that exits the pituitary. [Return to Figure 20.6].
Figure 20.7 image description: Part A of this figure is a diagram of the anterior view of the thyroid gland. The thyroid gland is a butterfly-shaped gland wrapping around the trachea. It narrows at its center, just under the thyroid cartilage of the larynx. This narrow area is called the isthmus of the thyroid. Two large arteries, the common carotid arteries, run parallel to the trachea on the outer border of the thyroid. A small artery enters the superior edge of the thyroid, near the isthmus, and branches throughout the two “wings” of the thyroid. Part B of this figure is a posterior view of the thyroid. The posterior view shows that the thyroid does not completely wrap around the posterior of the trachea. The posterior sides of the thyroid wings can be seen protruding from under the cricoid cartilage of the larynx. The posterior sides of the thyroid “wings” each contain two small, disc-shaped parathyroid glands embedded in the thyroid tissue. Within each wing, one disc is located superior to the other. These are labeled the left and right parathyroid glands. Just under the inferior parathyroid glands are two arteries that bring blood to the thyroid from the left and right subclavian arteries. Part C of this figure is a micrograph of thyroid tissue. The thyroid follicle cells are cuboidal epithelial cells. These cells form a ring around irregular-shaped cavities called follicles. The follicles contain light colored colloid. A larger parafollicular cell is embedded between two of the follicular cells near the edge of a follicle. [Return to Figure 20.7].
Figure 20.8 image description: This diagram shows the left adrenal gland located atop the left kidney. The gland is composed of an outer cortex and an inner medulla all surrounded by a connective tissue capsule. The cortex can be subdivided into additional zones, all of which produce different types of hormones. The outermost layer is the zona glomerulosa, which releases mineralcorticoids, such as aldosterone, that regulate mineral balance. Underneath this layer is the zona fasciculate, which releases glucocorticoids, such as cortisol, corticosterone and cortisone, that regulate glucose metabolism. Underneath this layer is the zona reticularis, which releases androgens, such as dehydroepiandrosterone, that stimulate masculinization. Below this layer is the adrenal medulla, which releases stress hormones, such as epinephrine and norepinephrine, that stimulate the symphathetic ANS. [Return to Figure 20.8].
Figure 20.9 image description: This diagram shows the anatomy of the pancreas. The left, larger side of the pancreas is seated within the curve of the duodenum of the small intestine. The smaller, rightmost tip of the pancreas is located near the spleen. The splenic artery is seen travelling to the spleen, however, it has several branches connecting to the pancreas. An interior view of the pancreas shows that the pancreatic duct is a large tube running through the center of the pancreas. It branches throughout its length in to several horseshoe- shaped pockets of acinar cells. These cells secrete digestive enzymes, which travel down the bile duct and into the small intestine. There are also small pancreatic islets scattered throughout the pancreas. The pancreatic islets secrete the pancreatic hormones insulin and glucagon into the splenic artery. An inset micrograph shows that the pancreatic islets are small discs of tissue consisting of a thin, outer ring called the exocrine acinus, a thicker, inner ring of beta cells and a central circle of alpha cells. [Return to Figure 20.9].
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.