4 Skill of Involvement
Learning Objectives
- Describe the types of intuition: holistic, affective, and inferential.
- Define empathy; how is empathy different from sympathy and empathy’s relationship to compassion?
- Define sensitivity; how does sensitivity in individuals impact clinical decision-making in nursing?
- Define cultural humility; how is cultural humility different from cultural competence?
Skill of Involvement
Skill of involvement (SOI) in nursing refers to higher-order holistic cognitive processes including intuition, empathy, sensitivity, and cultural humility that are recognized as holistic cognitive skills that can be measured and improved in nursing students (Benner et al., 2009). SOI enhances clinical decision-making and improves the delivery of person-centered care in all healthcare settings. Nurses utilizing SOI are needed now more than ever in a mechanized healthcare system that requires nursing to address healthcare equity by recognizing the impact of social determinants of health in diverse populations.
The increasingly technological environment in nursing has created a gap where the caring relationship between nurses and patients may suffer (Honkavuo & Abo, 2020). Nurse educators more than ever are responsible for providing presence, dialogue, intuition, creativity, and human interaction to students both in the classroom and online (Honkavuo & Abo, 2020). Consequently, these are the behaviors, qualities, traits, and cognitive skills that nurse educators would like to see in healthcare settings between students and patients. According to Benner et al. (2009), SOI is largely excluded currently in nursing education. There is a lack of language for SOI and a skilled social body of knowledge (Benner et al., 2009).
The American Association of Colleges (AACN) (2021) Essentials report speaks to clinical judgment, communication, compassionate care, diversity, ethics, evidence-based practice, health policy, and health equity as interwoven concepts across all of the nursing competency domains and are key elements required for nurses entering professional practice (AACN, 2021). Sub-competencies for entry-level professional nursing education within the domains point to SOI, such as ways of knowing (intuition), empathy, sensitivity and cultural humility, and individualized person-centered care in diverse populations delivered holistically with the intentional presence of the nurse (AACN, 2021).
Nurse educators can teach students to recognize intuition, empathy, sensitivity, and cultural humility as holistic cognitive skills that can be utilized with discernment alongside the nursing process to make clinical judgments in the provision of person-centered care that acknowledges SDOH. Furthermore, NCLEX-RN® alternative next-generation testing items are being incorporated into the licensure exam beginning in May of 2023 and item developers are using higher-order cognitive constructs for developing nursing clinical judgment alternative items that use a humanistic-intuitive model (Dickison, 2019).
Nurses who do not acquire SOI do not reach the level of expert nurses (Benner et al., 2009). Nursing students in the first year of education come to nursing with varying degrees of SOI which includes holistic cognitive processing skills, intuition type, levels of empathy, sensitivity, and cultural humility that can be measured, taught, and improved.
Nursing Is a Socially Embedded Practice
Nursing is a socially embedded practice (Benner et al., 2009). The skill of involvement includes holistic cognitive processes that most humans possess. Novice nurses lack experience in the clinical setting. Benner et al. (2009) state that novice nurses have “secondary ignorance and cannot know what they do not know” (p. 96). The novice nurse cannot rely on the salience obtained from practice that the proficient or expert-level nurse has gained.
There are human dimensions of the experience of illness that SOI uncovers through the presence of the patient. The human experience of illness cannot be completely “conveyed through decontextualized abstract labels or disengaged, analytical reasoning” (Benner et al., 2009). Skill of involvement uncovers the “patient story, meanings, intents, and concerns” (Benner et al., 2009, p. 211). The skill of involvement and life experience including experienced SDOH provide the nursing student with additional insight to guide clinical decision-making.
Implications for Basic Nursing Education
Benner et al. (2009) purport that a significant change in nursing education is needed and suggests that “as we help students learn clinical skills, they also must learn how to be with and take care of patients” (p. 370). Nursing students in undergraduate education need to understand how ethical principles translate to ethical comportment, as well as clinical decision-making that is informed by notions of good. “Sound clinical reasoning informed by the best available evidence and by a deep understanding of the patient’s concerns remain constant as the environment of care has been reinvented many times over” (Benner et al., 2009, p. 370).
The most recent statistics of new graduate nurses entering practice demonstrate a need for increased practice competency (Dickison, 2019; Kavanagh & Sharpnack, 2021). Nursing education is challenged to prepare new graduate nurses to enter practice with strong clinical decision-making skills. The focus on increasing students’ ability to make sound clinical decisions is at the forefront of concern in nursing education. Recognizing and analyzing cues with discernment in response to the patient’s condition and environment are emphasized as priority nursing assessments to support clinical decision-making and can be impacted by life experiences and SOI (Benner et al., 2009). The new NSCBN Clinical Judgement Model has been developed to “underscore the importance of investigating how nurse educators teach and measure nursing students’ abilities to make clinical judgments” (Dickison et al., 2019, p. 72).
Specifically, layer 3 depicts the cognitive processes used in clinical judgment and layer 4 includes factors of environment and factors of the individual (student). The model depicts the continuum of care from client needs to clinical decision-making in relation to the nursing process. Furthermore, the model can be utilized by educators in the design of simulation or test questions that link to specific cognitive skills that reflect the Intuitive-Humanistic Model and Dual Process Reasoning Model that link assessment of student critical thinking and rationale for clinical judgments (Dickison et al., 2019).
Figure 4-1
NCSBN Clinical Judgement Model
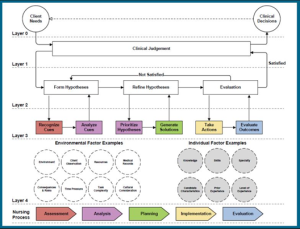
Note: (Dickison, 2019, n.p.).
Exploration of how the SDOH impacts SOI can assist new pre-licensure nursing students in navigating health inequality and holistically assessing patients through presencing in unfamiliar environments. Person-centered care requires holding patients in high regard, being sensitive to the environment, and providing care with ethical comportment and is necessary for nurses to attain the stage 5 expert level of nursing skill acquisition (Benner et al., 2010).
According to Price et al. (2017), “holistic, intuitive reasoning processes may be particularly valuable in the often complex and distracting environment of clinical care” (p. 1149). Nursing education that includes diversity, SDOH, cultural humility, and concepts of health equity will better prepare new graduates to provide person-centered care with improved clinical decision-making. These concepts can be “integrated and sustained throughout nursing school curricula and paired with community-based experiential opportunities whereby students can apply their knowledge, build their skills, and reflect on their experiences” (NASEM, 2021, p. 232).
Literature Review: Skill of Involvement and Clinical Judgment/Clinical Decision-Making
A smaller qualitative study was conducted by Dalton et al. (2018) to discover factors influencing clinical decision-making in nurses’ assessment and how nurses cognitively know and recognize when responding to acute patient deterioration. Newly qualified nurses with less than 2 years of experience and non-registered nurses were excluded from this sample, 10 nurses met the inclusion criteria. Demographic characteristics of the sample number of years in practice varied (n=3) 12 months or less, (n=3) 1-10 years, (n=2) 11-20 years, and (n=2) >20 years. Educational attainment certificate level (n=3), diploma level (n=3), and degree level (n=4). Even though this study did not include novice nurses or nursing students the findings are important to the study being proposed.
The data collection included taped recordings translated verbatim and much of the transcript is included in the journal article, and main themes and subthemes were identified. The main themes included: 1) collegial relationships with medical staff, 2) use of nursing intuition, 3) interpretation of the physiological parameter system, and the Modified Early Warning Score (MEWS). Subthemes further identified, a) clinical credibility, b) competence, c) confidence, d) expectation, e) knowledge, f) communication, g) leadership, h) legality, i) decision-making, j) organizational culture, and k) knowing the patient (Dalton et al., 2018, p. 217).
The findings are also discussed in the context of nursing history and socio-political history including gender and power hierarchy in the medical professions where nurse’s “assessment was mostly in the naturalistic domains of empirical works such as intuition and knowing the patient” and “medical staff rely on the defined systematic approach of assessment steeped in academic and empirical medical research” (Dalton et al., 2018, p. 215). Dalton et al. (2018) recognize intuition in nursing is a prominent theme and questions are raised for future research. Including, “do nurses really understand intuition” (p. 217)? The researchers further state, “Nurses would, arguably, be in a stronger position to validate the importance of their intuitive assumptions if they were to combine this with a knowledge base” (Dalton et al., 2018, p. 216). Nurses were more likely to not call the code team if assessment findings were more ambiguous, and more likely to request patient review when MEWs scores were high (Dalton et al., 2018). In this sense, the ‘‘nurses’ understanding would be increased and supplement their reasoning to persuade the medical team to review the patient” (Dalton et al., 2018, p. 218). The reluctance of nursing to discuss a personal view of a patient’s physiological decline with the parameters being so subtle, however, noticeable at the first instance asks where the “interpretation derived from: intuitive, experiential, theoretical or a mixture of all three” (Dalton et al., 2018, p. 2017)?
The findings from Dalton et al. (2018) correlate with Benners’ (2022) suggestion that skill of involvement is the relational engagement between nurse and patient, and discernment of the patient’s condition over time is paramount to strong clinical judgment and clinical decision-making. Benner (2022) discusses the skill of involvement as necessary to expert-level nursing and that it brings humanity, meaningfulness, acute situational awareness, and rapid thinking required for strong clinical decision-making in crisis management of the deteriorating patient. “While people are capable of reflective, deliberate conceptual thought, their most basic/primary access to the world is through emotional involvement, embodied skilled-knowing and social embeddedness in an already salient, meaningful world” (Benner, 2022, p. 2). Without the skill of involvement, we separate ourselves from the world which ultimately impedes our ability to connect with people, educators disconnect from students, and nurses disconnect from patients; this disconnect impedes decision-making in nursing (Benner, 2022). Benner (2022) points out that this “stance of separateness is particularly problematic in a profession that focuses on relationship and caring practice” (p. 2).
When nursing solely relies on critical rationality and analysis, the whole person is overlooked, and clinical decision-making requires looking at the nurses’ relation to attachment to outcome, specifically the “responsibility for the impact on the person(s), and situation(s) involved” (Benner, 2022, p. 3). Ways of knowing and human experience are essential to providing patient-centered care that considers the SDOH. Shared backgrounds, culture, and events increase concordance in healthcare. Intuition, empathy, sensitivity, and cultural humility are features/holistic cognitive skills that complement the science of nursing and are required to discern meaningfulness in nurse-patient interactions that prevent failure to rescue (Benner, 2022).
Skill of Involvement: Oklahoma Nursing Students
In Brown’s (2024) study Oklahoma Nursing student’s SOI mean scores on the TIntS subscales were highest overall in the use of inferential intuition type at 66.56%, affective intuition type at 57.25%, and holistic abstract intuition type at 51.54%. The highest proportion of nursing students in the sample are utilizing inferential intuition. Inferential intuition is domain-specific and seems to be utilized more based on gained experience or previous analytical processes that have become automatic (Dennin et al., 2021; Pretz et al., 2014). Affective intuition is based more on emotions or feelings and may rely more on gut feelings over analysis (Pretz et al., 2014). Holistic intuition is described as non-analytical and more abstract, thinking in theoretical terms, or noticing patterns (Dennin et al., 2022). The literature review uncovered that more experienced registered nurses would be expected to exhibit inferential intuition more prevalently than the other intuition types. The predominance of inferential intuition is an interesting finding in that first-year nursing students have little to no professional experience in a healthcare setting and are novice-level within the domain of nursing.
The IRI (empathy), HSPS (sensitivity), and CHI (cultural humility) instruments measured the participants’ level of empathy, sensitivity, and cultural humility. The higher the average score the higher the level of skill is possessed by the participant. Mean scores were reported as IRI 54.8% (61.39/112), HSPS 55.83% (46.9/84), and CHI 76.6% (72.8/95) demonstrating room for improvement in first-year nursing students to level up in each of the areas of SOI. Furthermore, HSPS, or being highly sensitive may be more of an innate trait rather than a skill that can be learned or improved (Pluess et al., 2023). Self-awareness of HSPS is important to the individual whether or not the cognitive trait or skill can be improved or not.
Intuition
There are three different types of intuition: holistic, inferential, and affective. Holistic intuition is characterized by a sense of knowing without being able to explain why. It’s like seeing the big picture without needing to analyze all the details. Inferential intuition is based on recognizing patterns and making quick judgments based on previous experiences. It’s like knowing the answer to a math problem without having to work through all the steps. Affective intuition is driven by emotions and feelings. It’s like having a gut feeling about something, even if you can’t logically explain it. All of these types of intuition can be helpful in nursing, but it’s important to be aware of their limitations. For example, affective intuition can be influenced by personal biases, so it’s important to check your gut feelings against objective data (Brown, 2024).
Empathy
Positive Impacts:
- Increased empathy and understanding: Sensitivity allows nurses to deeply connect with their patients, better understand their needs, and provide more compassionate care.
- Enhanced awareness of subtle changes in patient condition: Highly sensitive nurses may be more likely to notice slight changes in a patient’s vital signs, behavior, or emotional state that could signal a potential problem.
- Greater attention to detail: This can be beneficial in tasks such as medication administration or wound care, where precision and accuracy are essential.
- Overstimulation and stress: The demanding and often chaotic nature of healthcare environments can be overwhelming for highly sensitive individuals, leading to stress, burnout, and difficulty focusing.
- Emotional reactivity: While empathy is a valuable trait, excessive emotional reactivity can make it difficult for nurses to maintain professional boundaries and make objective decisions.
- Increased self-doubt and anxiety: Highly sensitive nurses may be more prone to second-guessing their decisions or feeling anxious about making mistakes, particularly in high-pressure situations.
|
Feature
|
Cultural Humility
|
Cultural Competence
|
|
Focus
|
Lifelong learning and self-reflection
|
Acquiring knowledge about specific cultures
|
|
Approach to difference
|
Openness, curiosity, and willingness to learn
|
Emphasis on understanding cultural norms and practices
|
|
Power dynamics
|
Acknowledges and seeks to mitigate power imbalances
|
May not explicitly address power dynamics
|
|
Goal
|
Mutually beneficial partnerships and patient-centered care
|
Culturally sensitive care based on knowledge of cultural differences
|
Note: Created with NotebookLM (Brown, 2024).
Reflection Questions:
Think about the four skills of involvement: intuition, empathy, sensitivity, and cultural humility. Which of these skills is most interesting to you? Why? Consider how you might use this skill when caring for patients. How might it help you provide better care?
- For example, if a student finds empathy most interesting, they might think about how they could use empathy to understand a patient’s fear or anxiety and provide emotional support.
Nursing is a “socially embedded practice.” What do you think this means? How do you think your own personal experiences and background will shape your skills of involvement as a nurse?
- For example, a student who has experienced social or economic hardship may have a deeper understanding of the challenges faced by patients from similar backgrounds. This understanding could enhance their ability to provide culturally sensitive care.
Glossary
- Clinical Decision-Making: The thought process nurses use to evaluate and choose the best course of action for a patient’s care. It is a complex process that involves critical thinking, analyzing patient data, considering evidence-based practices, and understanding the patient’s individual needs and preferences. Clinical decision-making is improved by SOI.
- Clinical Judgment: Similar to clinical decision-making, it refers to the ability of the nurse to make sound judgments about a patient’s condition and care needs, based on a combination of knowledge, experience, and intuition.
- Critical Rationality: A way of thinking that emphasizes logic and analysis, focusing on objective evidence and reasoning to reach conclusions. In nursing, relying solely on critical rationality can lead to overlooking the patient’s individual needs and experiences.
- Cultural Humility: The ability to recognize and respect the cultural differences between oneself and others. It involves being open to learning from patients about their cultural beliefs and practices, and incorporating this understanding into care.
- Empathy: The capacity to understand and share the feelings of another person. In nursing, empathy allows nurses to connect with patients on an emotional level, providing comfort and support.
- Expert Nurse: A nurse who has achieved a high level of skill and knowledge through experience and continued learning. Expert nurses are able to make complex clinical judgments quickly and effectively, and are often sought out as mentors by other nurses.
- Failure to Rescue: A term used to describe a situation where a patient’s condition deteriorates, and the healthcare team fails to recognize and respond appropriately, potentially leading to serious complications or death. SOI can help prevent this.
- Holistic Cognitive Skills: Mental abilities that involve considering the whole person, including their physical, emotional, social, and spiritual needs. These skills are essential for providing patient-centered care that addresses the individual’s unique circumstances.
- Intuition: A form of knowledge that comes from instinct or feeling, rather than from conscious reasoning. In nursing, intuition can help nurses to quickly assess situations and make decisions, even when there is limited information available.
- Novice Nurse: A nurse who is new to the profession and is still developing their skills and knowledge. Novice nurses often rely on rules and procedures to guide their practice, and may need more time and support to make clinical decisions.
- Person-Centered Care: A philosophy of care that places the patient at the center of all decision-making. It emphasizes respect for the individual’s values and preferences, and strives to provide care that is tailored to their specific needs.
- Sensitivity: The ability to perceive and respond to subtle cues in the environment and in others. In nursing, sensitivity allows nurses to pick up on nonverbal communication, recognize changes in a patient’s condition, and anticipate their needs.
- Skill of Involvement (SOI): Holistic thinking processes that involve a nurse’s intuition, empathy, sensitivity, and cultural humility. SOI is a skill that can be learned and improved in nursing school and in practice.
NCLEX Practice Questions
Question 1
A novice nurse asks her preceptor about the concept of “skill of involvement” (SOI) in nursing. Which response by the preceptor is the most accurate?
a) “SOI is a skill that can only be learned through years of experience.”
b) “SOI primarily focuses on technical skills and medical knowledge.”
c) “SOI is not relevant to novice nurses as they lack experience.”
d) “SOI involves holistic cognitive skills like intuition, empathy, and cultural humility.”
Question 2
A nursing student is caring for a patient from a different cultural background. The student feels unsure about how to approach the patient’s spiritual needs. What would be the most appropriate action for the student to take?
a) Avoid discussing spirituality to prevent causing offense.
b) Assume the patient’s spiritual needs based on their religion.
c) Consult a textbook for information on the patient’s specific culture.
d) Respectfully ask the patient about their spiritual beliefs and practices.
Question 3
A new graduate nurse is feeling overwhelmed by the demands of the job and is questioning their ability to provide competent care. Which statement reflects a lack of skill of involvement (SOI) that could hinder the nurse’s clinical judgment?
a) “I need to carefully analyze patient data and follow protocols to ensure safe care.”
b) “I should seek guidance from experienced nurses when I’m uncertain about a situation.”
c) “My gut feeling is telling me something is wrong, but the vital signs are stable.”
d) “I’m afraid to make a mistake, so I’m only focusing on the tasks and not the patient.”
Question 4
Which scenario best exemplifies a nurse demonstrating the skill of involvement (SOI) in clinical practice?
a) A nurse efficiently administers medications to all patients on time according to the MAR.
b) A nurse recognizes a subtle change in a patient’s breathing pattern and promptly notifies the physician.
c) A nurse delegates tasks to unlicensed assistive personnel (UAP) to manage time effectively.
d) A nurse uses a standardized assessment tool to collect patient data during the admission process.
Question 5
According to the sources, what is a potential consequence for nurses who do not develop skill of involvement (SOI)?
a) They may have difficulty adapting to new technologies in healthcare.
b) They may be less likely to advance to the level of expert nurse.
c) They may experience higher levels of job satisfaction and burnout.
d) They may struggle to meet the minimum competency requirements for licensure.
Question 6
The NCSBN Clinical Judgment Model highlights the importance of considering “factors of the individual” when making clinical decisions. Which example best reflects this concept?
a) A nurse adjusts pain management strategies based on the patient’s cultural beliefs about pain expression.
b) A nurse uses evidence-based guidelines to determine the appropriate dose of medication for a patient.
c) A nurse follows hospital policy when administering blood transfusions to ensure patient safety.
d) A nurse uses a clinical decision support system to help interpret a patient’s laboratory results.
References:
American Association of Colleges of Nursing (AACN). (2021). The Essentials: Core competencies for professional nursing education.https://www.aacnnursing.org/Portals/0/PDFs/Publications/Essentials-2021.pdf
Benner, P. (2022). Overcoming Descartes’ representational view of the mind in nursing pedagogies, curricula, and testing. https://doi.org/10.1111/nup.12411
Benner, P., Sutphen, M., Leonard, V., & Day, L. (2010). Educating nurses: A call for radical transformation. Jossey-Bass.
Benner, P., Tanner, C., & Chesla, C. (2009). Expertise in Nursing Practice: Caring, clinical judgment, and ethics. Springer.
Brown, Cynthia, “Impact of Social Determinants of Health on Skill of Involvement: Differences in First Year ADN and BSN Nursing Students in Rural Oklahoma” (2024). Dissertations. 2230. https://aquila.usm.edu/dissertations/2230
Dalton, M., Harrison, J., Malin, A., & Leavey, C. (2018). Factors that influence nurses’ assessment of patient acuity and response to acute deterioration. British Journal of Nursing, 27(4):212-218. https://doi.org/10.12968/bjon.2018.27.4.212
Dennin, A., Furman, K., Pretz, J. E., & Roy, M. M. (2022). The relationship of types of intuition to thinking styles, beliefs, and cognitions. Journal of Behavioral Decision Making, 35(5), e2283. https://doi.org/10.1002/bdm.2283
Dickison, P. D. (2019). NCSBN and the Next Generation NCLEX. NCSBN.https://www.aacnnursing.org/portals/0/PDFs/Conferences-Webinars/Presentations/2019/dickison-presentation.pdf
Honkavuo, L. & Abo, R. (2020). Digital teaching in nursing education: A quantitative study on nursing students’ views. International Journal of Caring Sciences, 13(2), 837-846. https://www.internationaljournalofcaringsciences.org/docs/8_1_honkauvo_original_13_2.pdf
National Academies of Sciences, E., & Medicine (NASEM). (2021). The Future of Nursing 2020-2030: Charting a Path to Achieve health Equity. (M. K. Wakefield, D. R. Williams, S. Le Menestrel, & J. L. Flaubert, Eds.). National Academies Press. https://doi.org/10.17226/25982
Pluess, M., Lionetti, F., Aron, E., & Aron, A. (2023). People Differ in their Sensitivity to the Environment: An Integrated Theory, Measurement and Empirical Evidence. Journal of Research in Personality. https://doi.org/10.1016/j.jrp.2023.104377
Pretz, J., Brookings, J., Carlson, L., Humbert, T., Roy, M., Jones, M., & Memmert., D. (2014). Development and validation of a new measurement. Journal of Behavioral Decision Making, 27(5), 454-467. https://doi-org.lynx.lib.usm.edu/10.1002/bdm.1820
Price, A., Zulkosky, K., White, K., & Pretz, J. (2017). Accuracy of intuition in clinical decision-making among novice clinicians. Journal of Advanced Nursing, 73(5), 1147-1157. https://pubmed.ncbi.nlm.nih.gov/27862180/