11 Holistic Nursing Process: Humanizing Healthcare
Learning Objectives
- Explain the concept of humanizing healthcare and analyze how addressing SDOH contributes to a more humanized and equitable healthcare system.
- Apply the holistic nursing process model, incorporating SOI and SDOH considerations, to a patient case study.
- Explain the importance of a diverse nursing workforce and identify strategies for promoting diversity and inclusion in healthcare.
Welcome to the final chapter of this textbook! Here, we will explore a crucial topic that weaves together all the knowledge and skills you’ve learned so far: humanizing healthcare. This chapter goes beyond clinical expertise and delves into the heart of nursing–building meaningful connections with patients and communities while advocating for a more just and equitable healthcare system.
The Power of Understanding: Social Determinants of Health in Nursing
As nurses, we are more than just caregivers; we are advocates, educators, and changemakers. To truly embody this role, we must recognize the powerful forces shaping our patients’ lives and health outcomes. These forces, known as the social determinants of health (SDOH) encompass the conditions in which people are born, grow, live, work, and age. Imagine a tapestry woven with threads representing economic stability, education access and quality, neighborhood and built environment, healthcare access and quality, and social and community context. These threads intertwine to create the unique circumstances of each individual’s life.
By understanding the SDOH, we gain a deeper understanding of our patients’ stories. We can move beyond treating symptoms and address the root causes of health inequities. This knowledge empowers us to provide holistic care that considers the whole person– their physical, emotional, social, and spiritual well-being (Perez, 2019).
Holistic Nursing Process: Humanizing Healthcare
In an era defined by rapidly evolving technology, it is more crucial than ever to re-center the human experience in healthcare. This chapter, explores the essential yet often overlooked aspects of nursing that go beyond technical skills and embrace the holistic needs of each individual. Two fundamental concepts that are integral to humanizing healthcare: Skill of Involvement (SOI) and Social Determinants of Health (SDOH) are linked to the nursing process. As healthcare increasingly relies on technology and data-driven approaches, the risk of depersonalization and a disconnect between providers and patients becomes more pronounced. Nursing, as the profession most directly involved in patient care, has a unique responsibility to bridge this gap and ensure that the human connection remains at the heart of healthcare.
The concept of SOI, encompasses the holistic cognitive processes that nurses utilize to connect with patients on a deeper level. SOI includes elements of intuition, empathy, sensitivity and cultural humility. By cultivating SOI, nurses can provide care that is not only clinically competent but also deeply humanizing. The SDOH encompasses the social, economic, and environmental factors that influence health outcomes. These factors, which range from access to quality education and safe housing to experiences of discrimination and social isolation, have a profound impact on an individual’s well-being and ability to achieve optimal health.
Nurse educators play a vital role in promoting workforce innovation by equipping future nurses with the knowledge and skills to address the SDOH and provide equitable care to diverse populations. This necessitates a commitment to diversity and inclusion within the nursing workforce, recognizing that a more diverse group of nurses will be better equipped to understand and respond to the unique needs of their patients.
The following sections of this chapter will provide nurse educators with a deeper understanding of SOI and SDOH and explore practical strategies for integrating these concepts into nursing education. We will emphasize the importance of workforce innovation through diversity and inclusion as essential to providing humanized and equitable healthcare for all.
Figure 11-1 Theoretical Framework
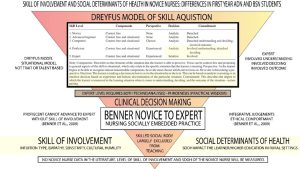
Note: (Brown, 2024)
Building on the concept of Skill of Involvement (SOI) and recognizing the profound impact of Social Determinants of Health (SDOH), this chapter proposes a paradigm shift in nursing education by introducing a holistic nursing process model. This model, illustrated in Figure 11-2, goes beyond the traditional steps of assessment, diagnosis, planning, intervention, and evaluation by explicitly integrating SOI and SDOH into each phase of the nursing process.
At the heart of this model is the recognition that nursing is both an art and a science. The “art” of nursing is embodied in SOI, encompassing the nurse’s intuition, empathy, sensitivity, and cultural humility. These qualities, honed through experience and self-reflection, enable nurses to connect with patients on a deeper level, understand their unique needs and perspectives, and provide truly patient-centered care. The “science” of nursing is grounded in evidence-based practice, critical thinking, and clinical judgment. The holistic model seamlessly blends these two aspects, recognizing that optimal patient outcomes are achieved when clinical expertise is combined with compassionate, humanized care.
The model also highlights the critical role of SDOH in influencing a patient’s health and well-being. By explicitly considering the social, economic, and environmental factors that impact a patient’s life, nurses can develop care plans that are more comprehensive and responsive to their individual needs. This approach aligns with the core competencies for nursing education outlined in the American Association of Colleges (AACN) Essentials report which emphasizes clinical judgment, compassionate care, diversity, ethics, and health equity (AACN, 2021). The model further underscores the importance of ethical comportment, duty to care, and creative discernment as guiding principles for nurses in navigating the complexities of healthcare delivery. Ultimately, this holistic nursing process model aims to cultivate a new generation of nurses who are not only skilled clinicians but also compassionate advocates for their patients, committed to providing equitable and humanized care for all.
Figure 11-2 Holistic Nursing Process
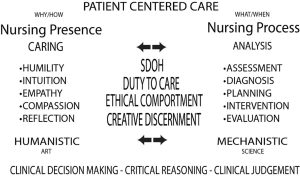
Note: (Brown, 2024)
Case Study: Maria Hernandez
Setting: A busy urban hospital, medical-surgical unit.
Characters:
- You: A new graduate nurse (RN) beginning your first job on a medical-surgical unit.
- Maria Hernandez: A 58-year-old woman admitted for uncontrolled diabetes and a foot ulcer.
- Preceptor: An experienced RN assigned to mentor you.
Clinical Scenario:
Shift Start: You are eager to begin your first shift as a registered nurse. You meet your preceptor, a seasoned nurse known for her patient-centered approach. She introduces you to Maria Hernandez, your assigned patient.
Initial Assessment: As you begin your assessment, your preceptor emphasizes the importance of the holistic nursing process, integrating Skill of Involvement (SOI) and considering the Social Determinants of Health (SDOH) that may be influencing Maria’s current health status. You review Maria’s medical chart, noting her history of diabetes, hypertension, and a recent non-healing ulcer on her right foot.
Applying SOI: You enter Maria’s room and introduce yourself. Taking time to connect with her, you practice your SOI skills:
- Intuition: You notice that Maria seems withdrawn and hesitant to make eye contact. You sense she may be anxious or overwhelmed.
- Empathy: You acknowledge that it must be difficult to be hospitalized, especially with a complicated health condition.
- Sensitivity: You adjust your communication style, speaking softly and using simple language. You ensure Maria feels heard and respected.
- Cultural Humility: You are mindful of Maria’s Hispanic heritage and inquire about any cultural preferences or beliefs that might affect her care.
Uncovering the Story: As you gently assess Maria’s foot ulcer, you ask about her ability to manage her diabetes at home. Maria shares that she lives in a small apartment with her daughter and two grandchildren. She recently lost her job at a local factory and is struggling to afford healthy food and her medications. She explains that her neighborhood lacks safe places to exercise, and she often feels isolated.
Recognizing the SDOH: You realize Maria’s challenges extend far beyond her physical health. You recognize the powerful influence of SDOH on her well-being. Specifically:
- Economic Stability: Job loss and financial strain limit her access to healthy food and medication.
- Neighborhood and Built Environment: Lack of safe spaces for exercise impacts her ability to manage her diabetes.
- Social and Community Context: Social isolation and potential language barriers create additional challenges.
Developing the Care Plan:
Diagnosis: In addition to her medical diagnoses, you identify several nursing diagnoses related to Maria’s SDOH, such as: Risk for unstable blood glucose levels related to financial constraints and Social Isolation related to limited community resources and language barriers.
Planning: You collaborate with Maria, recognizing her as an active participant in her care. You involve the social worker to connect her with resources for food assistance and affordable medications. You also explore transportation options to a community center with diabetes support groups and exercise programs.
Intervention: You provide patient education on diabetes management, emphasizing realistic strategies given Maria’s circumstances. You encourage her to connect with the support groups and explore community resources.
Evaluation: You recognize the importance of ongoing evaluation, recognizing that Maria’s needs and circumstances may evolve. You work with Maria to assess the effectiveness of the interventions and make adjustments as needed.
Reflecting on the Experience:
At the end of your shift, you debrief with your preceptor. You discuss how the holistic nursing process, guided by SOI and a deep understanding of SDOH, allowed you to develop a truly patient-centered care plan for Maria. You realize that humanizing healthcare means seeing the person behind the diagnosis, recognizing the unique tapestry of their lives, and empowering them to achieve their highest level of well-being. You are proud to be a part of a profession that advocates for a more just and equitable healthcare system. This case study illustrates the importance of integrating the holistic nursing process, including SOI and SDOH considerations, into patient care. It highlights the role of the novice nurse in developing patient-centered care plans that address the whole person, not just their physical symptoms.
Putting it All Together: Applying Holistic Nursing and Humanizing Healthcare
Holistic nursing is the cornerstone of humanizing healthcare. It is about seeing the person behind the diagnosis, recognizing their unique experiences, and providing individualized care (NASEM, 2016). By integrating our understanding of SDOH into the holistic nursing process, we can assess and address the impact of these factors on our patients’ overall well-being.
Your Journey Begins: Strategies for Nursing Students
As you embark on your nursing journey, consider these strategies:
Engage in Self-Reflection: Take time to reflect on your own biases and assumptions about individuals and communities. This self-awareness helps you provide unbiased, culturally sensitive care.
Embrace Experiential Learning: Actively seek opportunities to learn in diverse community settings. These experiences will enrich your understanding of the real-world impact of SDOH.
Seek Collaboration: Surround yourselves with nurses and other healthcare professionals from diverse backgrounds. Learn from their experiences, insights, and knowledge.
Be an Advocate: Use your voice to advocate for policies and practices that promote health equity and address the SDOH. You have the power to influence positive change in healthcare systems.
You are entering a profession that is deeply intertwined with the lives of individuals and communities. By embracing diversity, understanding the SDOH, and advocating for equity, you will be an integral part of creating a more humanized and compassionate healthcare system.
Implications for Nursing Education
Building a Better Future: Nursing Education and Workforce Innovation
Nursing education is the foundation upon which we build our practice. To create a more humanized healthcare system, we must embrace innovative approaches to nursing education that equip nurses with the knowledge, skills, and values needed to address the SDOH (NASEM, 2016).
- Transformative Learning: Picture a caterpillar transforming into a butterfly. Transformative learning takes us beyond a traditional biomedical focus to develop a deeper understanding of complex health systems in an interconnected world. It is about becoming enlightened change agents, skilled in analyzing healthcare systems, advocating for policies, and collaborating with communities (NASEM, 2016).
- Experiential Learning: Learning isn’t confined to the classroom! Experiential learning encourages you to immerse yourselves in diverse community settings and witness the real-world impact of SDOH. This hands-on experience, combined with thoughtful reflection, allows you to challenge your assumptions and grow as future nurses (NASEM, 2016).
- Collaborative Learning: Collaboration is at the heart of nursing. Collaborative learning emphasizes teamwork and interprofessional collaboration to address SDOH effectively. By working together, we can create innovative solutions and advocate for our patients and communities (NASEM, 2016).
- Integrated Curricula: Integrated curricula connect different aspects of nursing education, blending theory and practice. They provide opportunities for interprofessional learning, allowing nursing students to learn alongside students from other health professions and gain a broader perspective on SDOH (NASEM, 2016).
- Continuing Professional Development: Learning doesn’t stop after graduation. Continuing professional development (CPD) helps nurses stay updated on the latest research and best practices in addressing SDOH (NASEM, 2016).
Breaking Down Barriers: Recognizing Structural Barriers to Education
We must acknowledge that not everyone has equal opportunities to pursue a nursing education. Structural barriers, like socioeconomic disparities, discrimination, and limited access to resources, can hinder individuals from reaching their full potential (NASEM, 2016). As advocates for equity, we must actively support programs that address these barriers and champion equitable access to education for all.
Celebrating Our Differences: The Importance of Diversity in Healthcare
A diverse nursing workforce is essential for providing culturally competent and equitable care (NASEM, 2016). Imagine a healthcare system where nurses reflect the diverse communities they serve, creating a space of understanding and trust. This includes diversity in race, ethnicity, language, socioeconomic background, sexual orientation, gender identity, and disability.
When patients see themselves reflected in their healthcare providers, it fosters a deeper connection and improves communication (NASEM, 2016). Research shows that racial/ethnic concordance between patients and providers leads to greater trust, shared decision-making, and ultimately, better health outcomes (Perez et al., 2019). We must actively work towards recruiting, retaining, and supporting a diverse nursing workforce and faculty.
Glossary:
Collaborative Learning: A style of learning that prioritizes teamwork and working with other healthcare professionals to solve problems related to the social determinants of health.1
Continuing Professional Development (CPD): Continued learning and development in the field of nursing that occurs after graduation. This helps nurses keep their knowledge and skills up to date, especially regarding information about social determinants of health.
Experiential Learning: A hands-on learning style that allows nursing students to learn in real-world settings. This type of learning is important for understanding how social determinants of health affect people and communities in diverse settings.
Holistic Nursing: A nursing practice that goes beyond treating symptoms and considers the patient’s physical, emotional, social, and spiritual well-being to provide individualized care.
Holistic Nursing Process: A model of nursing that explicitly integrates skill of involvement and social determinants of health into every step of the nursing process (assessment, diagnosis, planning, intervention, and evaluation).
Humanizing Healthcare: Providing healthcare that is centered on the patient’s experience and considers their needs and perspectives, beyond just clinical care.
Integrated Curricula: A style of curriculum that combines different nursing topics, theory, and practical application and provides interprofessional learning opportunities for students to learn from each other.
Structural Barriers: Systemic obstacles like socioeconomic disparities, discrimination, and lack of resources that can prevent some people from getting a nursing education.
Transformative Learning: A type of learning that encourages nurses to move beyond a solely biomedical approach and develop a deeper understanding of the complexities of healthcare systems.
References:
Brown, Cynthia, “Impact of Social Determinants of Health on Skill of Involvement: Differences in First Year ADN and BSN Nursing Students in Rural Oklahoma” (2024). Dissertations. 2230.https://aquila.usm.edu/dissertations/2230
National Academies of Sciences, Engineering, and Medicine (NASEM). (2016). A framework for educating health professionals to address the social determinants of health. The National Academies Press. https://doi.org/10.17226/21923
Perez, A. G., Mertz, L., Brassard, A., Alvarez, C., Williams, E. J., Smith, B. K., Littlejohn, S., Cuellar, N., Dawson, M., Joy Garcia-Dia, M., consultants Kupiri Ackerman-Barger, committee, Eddie, R., Martin, L., & Nichols, B. (2019). A literature scan and framework of a diverse nursing workforce and its effect on the social determinants of health We appreciate the review and contributions of the Campaign for Action’s Equity, Diversity, and Inclusion Steering Committee. Future of Nursing: Campaign for Action at the Center to Champion Nursing in America. https://campaignforaction.org/